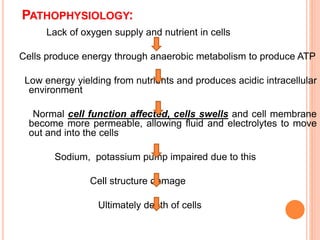
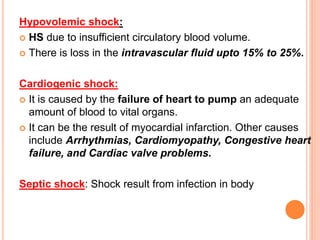
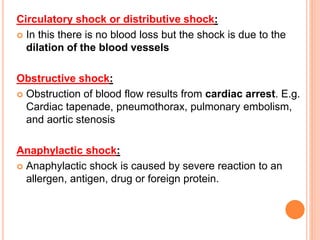
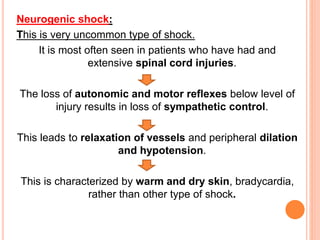
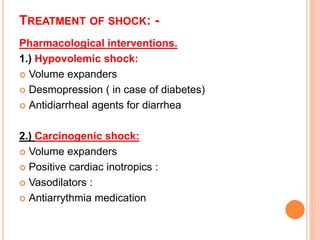
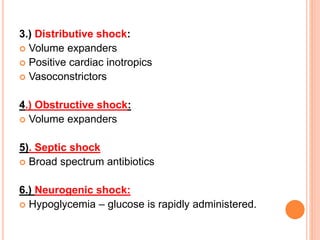
This document discusses shock, its causes, pathophysiology, classification, stages, signs and symptoms, diagnosis, treatment and nursing management. Shock is defined as a life-threatening condition characterized by inadequate tissue perfusion. It can result from reduced blood volume, heart malfunction, lung issues, or other causes. Shock progresses through compensatory, progressive and irreversible stages. Treatment involves restoring blood volume, increasing cardiac output, treating underlying causes, and supportive nursing care.