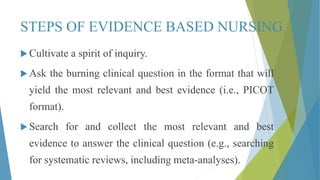
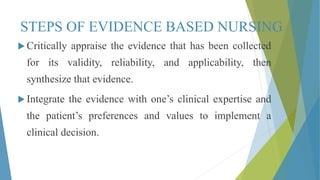
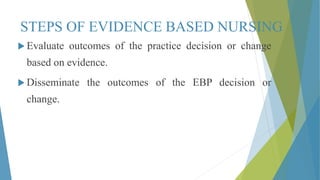
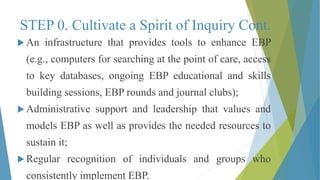
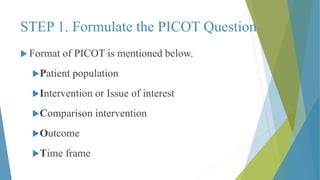
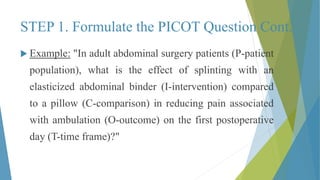
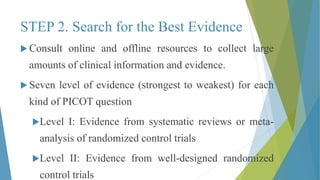
This document defines evidence-based nursing and its key components. Evidence-based nursing integrates the best research evidence, clinical expertise, and patient values and preferences. It involves cultivating a spirit of inquiry, asking clinical questions, searching for evidence, critically appraising evidence, integrating evidence with expertise and patient preferences, evaluating outcomes, and disseminating results. Barriers to evidence-based nursing include lack of skills/time and organizational constraints, while supports include leadership, resources, and mentors.