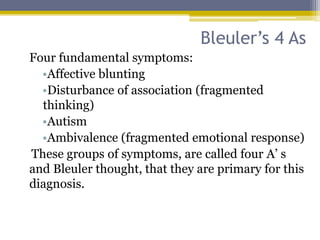
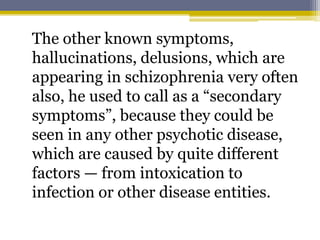
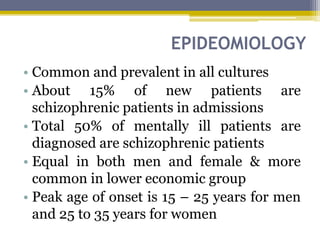
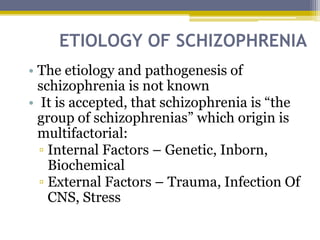
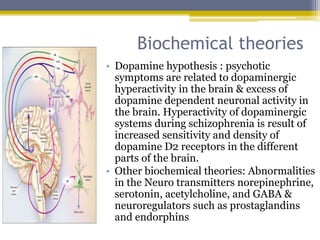
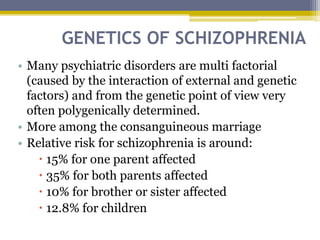
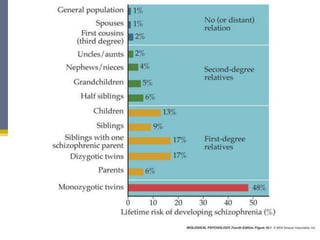
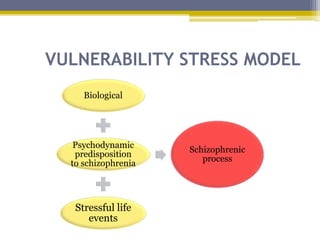
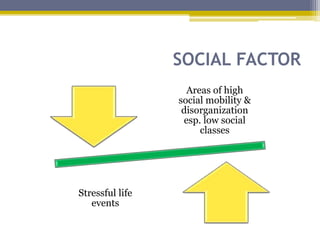
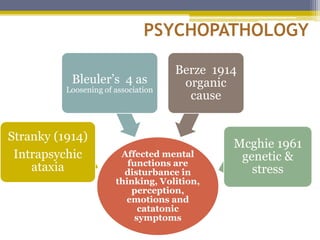
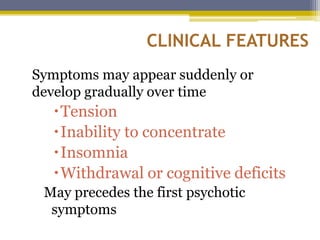
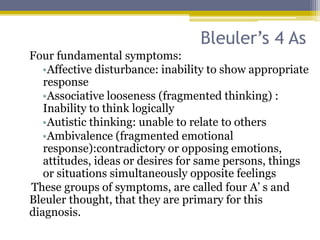
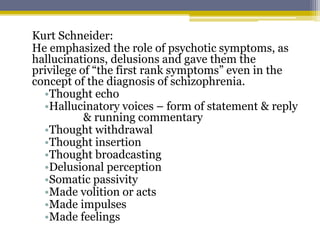
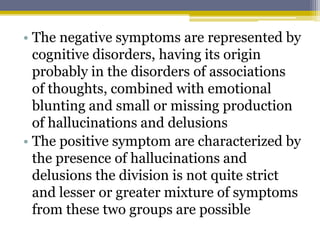
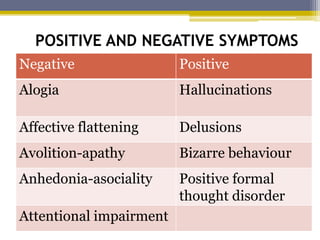
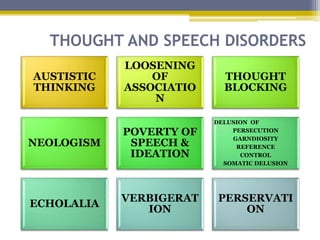
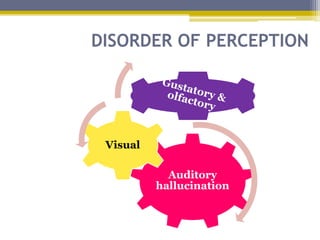
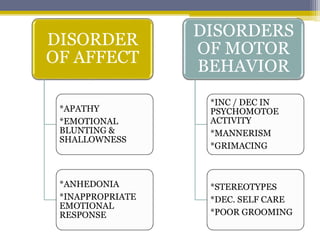
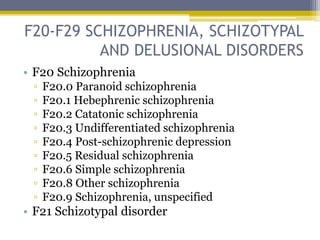
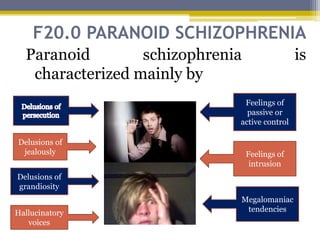
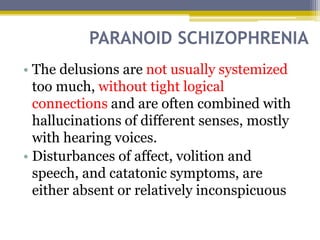
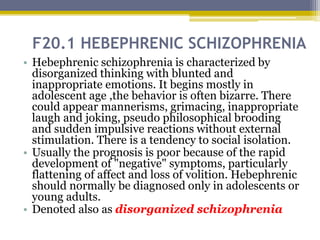
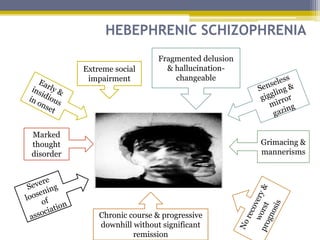
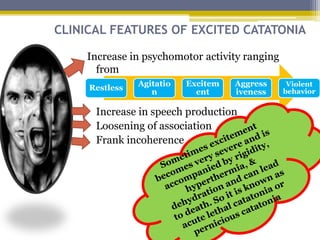
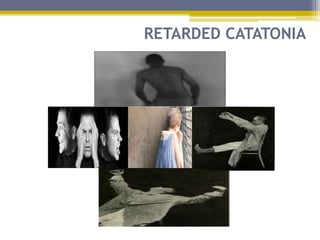
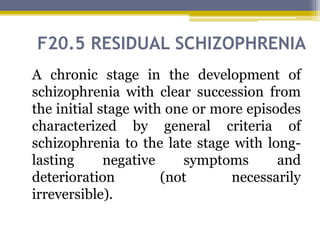
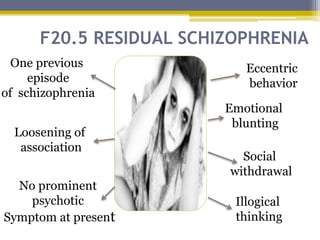
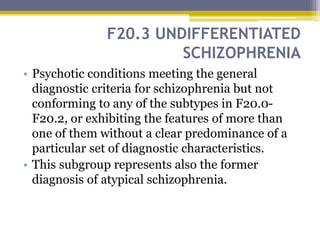
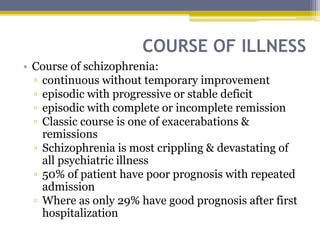
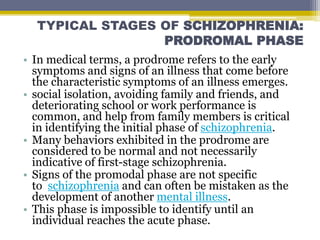
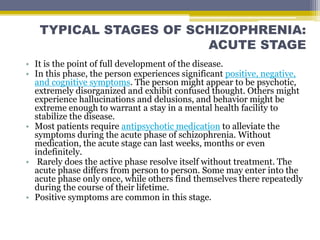
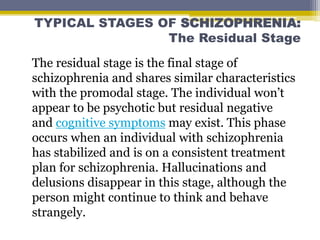
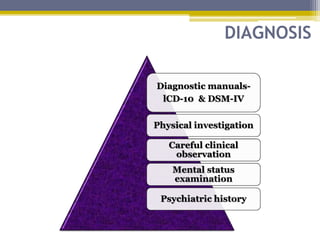
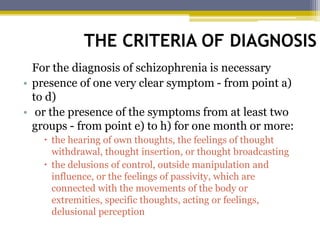
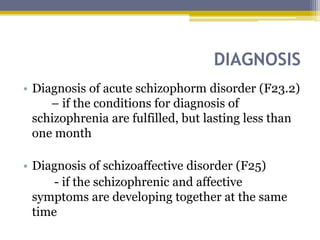
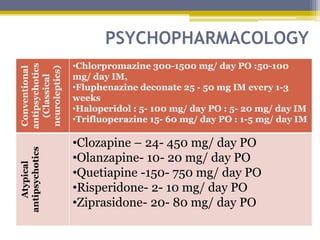
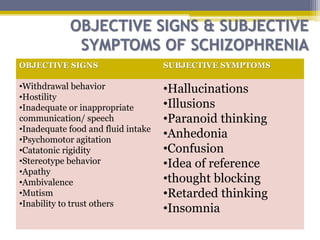
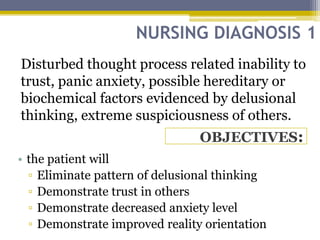
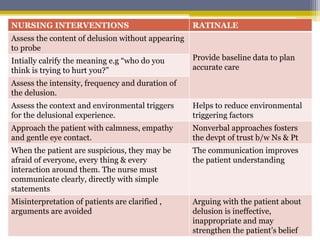
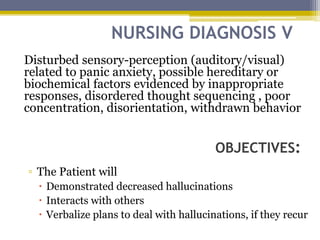
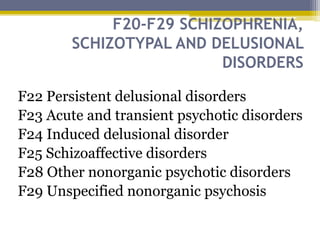
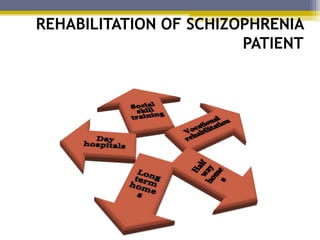
Schizophrenia is a psychotic disorder characterized by distortions in thinking, perception, emotions, and behavior, with an onset typically between ages 15-25. The etiology is multifactorial, involving genetic, biochemical, and environmental factors, and it presents with both positive and negative symptoms including hallucinations and emotional blunting. Treatment primarily involves antipsychotic medications and psychological therapies to manage symptoms and support rehabilitation.