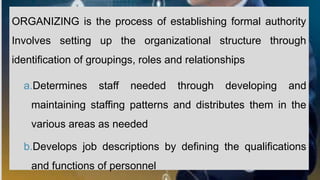
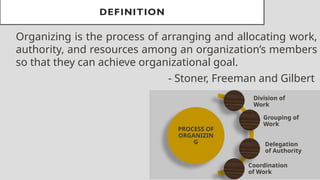
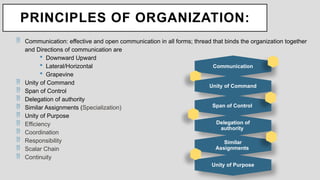
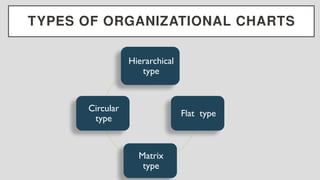
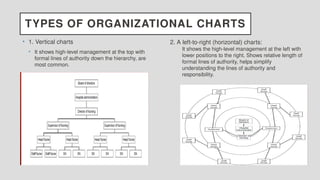
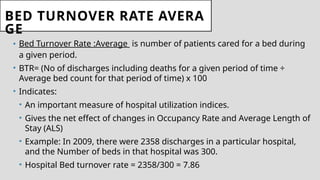
The document provides a comprehensive overview of organizational management within the nursing sector, detailing processes such as organizing, hospital administration, and effectiveness assessment. It discusses various organizational structures, their advantages and disadvantages, and emphasizes the importance of communication, authority, and resource management in achieving healthcare goals. Additionally, it covers hospital statistics and key performance indicators that evaluate hospital utilization and service quality.



































![BED OCCUPANCY RATE (BOR)
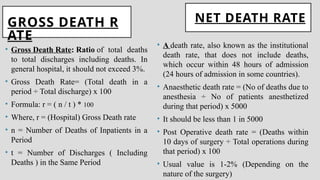
• BOR is the average occupancy of hospital beds in
percentage. It is the ratio between beds used and beds
provided.
• The beds occupancy rate is calculated based on the
midnight bed census at each hospital.
• Number of patients' day (service days) in a year =
Number of beds x 365 X 100
• [For example, the BOR for Monday is based on the bed census taken at 0000 hrs
Tuesday].
• - 80-85% BOR is ideal for good quality of patient care.
• - 15-20% beds are vacant for emergency, maternity, isolation, intensive care (Dead](https://image.slidesharecdn.com/organizing-241214183037-114798d5/85/ORGANIZING-IN-NURSING-MANAGEMENT-POWERPOINT-52-320.jpg)