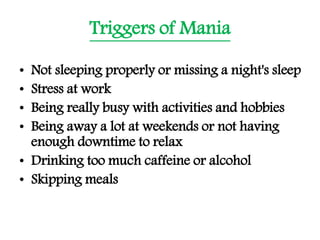
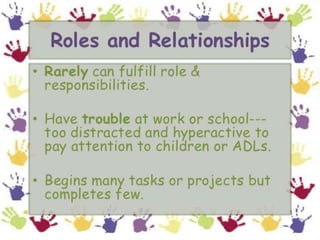
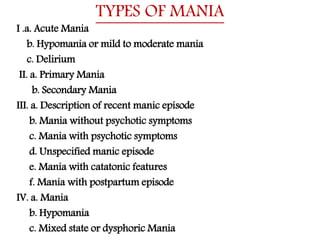
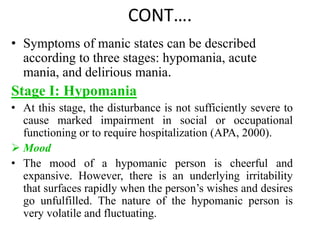
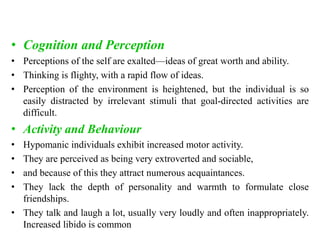
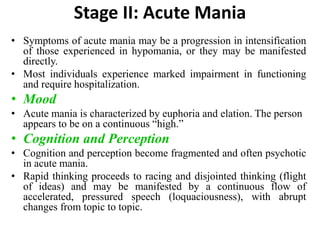
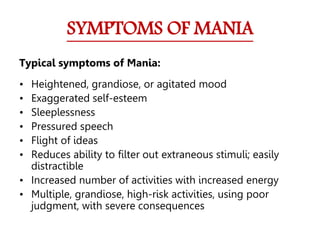
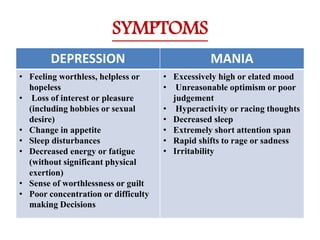
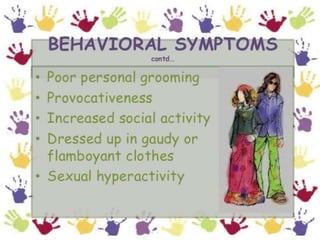
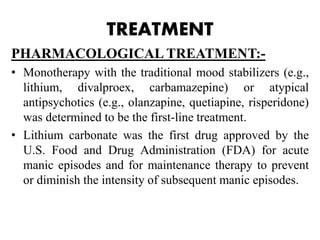
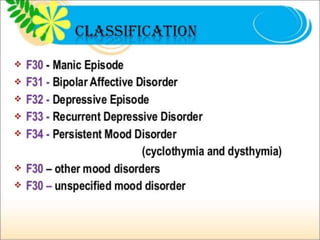
The document discusses mood disorders, which include major depression, bipolar disorder, and dysthymia, highlighting their symptoms, incidence, and socio-economic impact. It describes the characteristics of manic episodes, stages of mania, and treatment options including pharmacological and therapeutic approaches. Additionally, it emphasizes the importance of safety, appropriate behavior management, and self-care in nursing interventions for individuals with mood disorders.
![Normal Vs. Pathological Mood
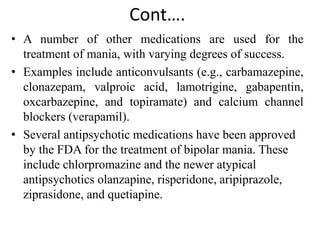
SL.
NO
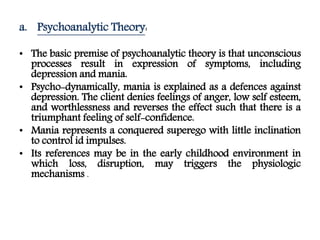
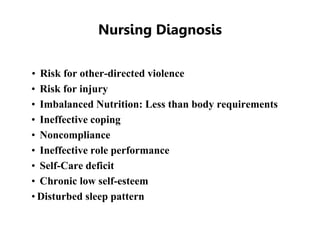
FEATURES NORMAL MOOD PATHOLOGICAL MOOD
1 BODY
FUNCTIONS
NORMAL BODILY
FUNCTIONS[ E.g.
adequate sleep, appetite]
IMPAIRMENTS OF BODY FUNCTIONS
[e.g. disturbances in sleep, appetite, sexual
interest, gastro intestinal activity]
2 SOCIAL ROLES WELL SOCIALISED
PERFORM ALL THE
EXPECTED ROLES
REDUCED DESIRE AND ABILTY TO
PERFORM USUAL EXPECTED ROLES
[e.g. family responsibilities, at work, in
school]
3 SUICIDEAL
IDEATIONS
SUICIDAL THOUGHTS
OR ACTS ABSENT
SUICIDAL THOUGHTS OR ACTS
PRESENT
4 REALITY
TESTING
NORMAL REALITY
TESTING[ No delusion,
hallucination, confusion
present]
DISTRUBANCES IN REALITY
TESTING[e.g. delusions present,
hallucinations, confusion present]](https://image.slidesharecdn.com/mooddisorderme-190928054614/85/Mood-disorder-7-320.jpg)
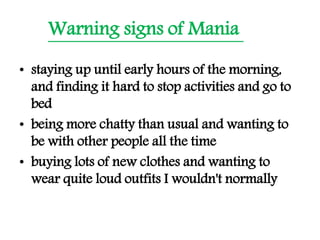
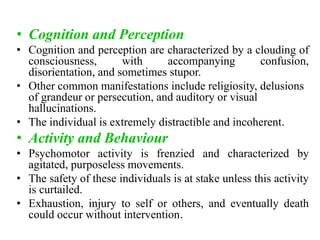
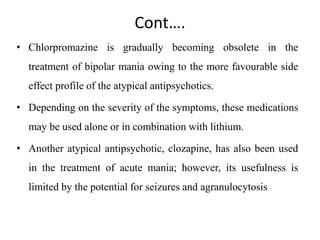
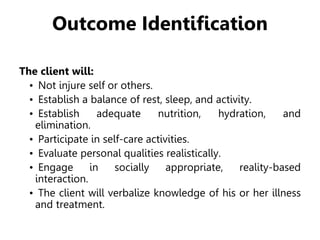
![STAGES OF MANIA
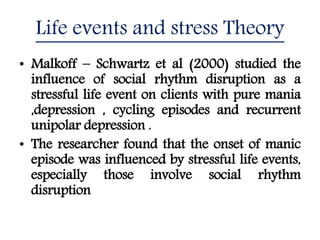
STAGE – I [EUPHORIA ] STAGE – II [ELATION] STAGE – III [EXALTATION]
MOOD Liability of affect,
euphoria predominates,
irritability if demands
not satisfied.
Increased dysphoria
and depression, open
hostility and anger
Clear dysphoric , panic
stricken hopeless
COGNITION Expansive, grandiosity,
over-confidence,
thoughts coherent, but
occasionally tangential
, sexual and religious
pre-occupation. Racing
of thoughts
Flight of ideas,
disorganization of
cognitive state,
delusions
Incoherent, definite
loosening of association,
bizarre and idio –
syncratic delusions,
hallucinations in one –
third of the patients,
occasional ideas of
reference .
BEHAVIOR Increased psychomotor
activity, increased
initiation and rate of
speech, increased
spending, smoking,
telephone use.
Continued increased
psychomotor
acceleration, increased
pressured speech,
occasional assaultive
behaviour.
Frenzied and frequently
bizarre psychomotor
activity.](https://image.slidesharecdn.com/mooddisorderme-190928054614/85/Mood-disorder-15-320.jpg)