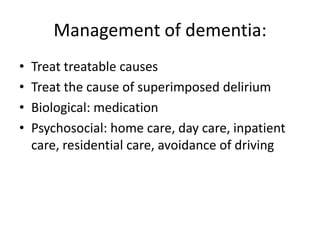
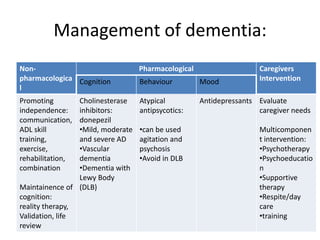
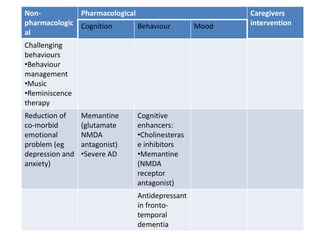
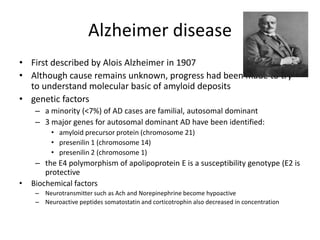
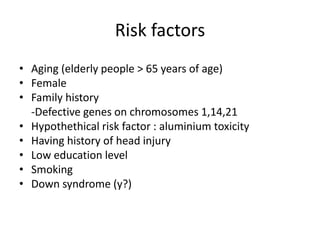
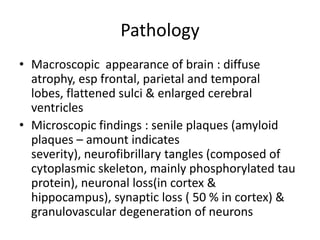
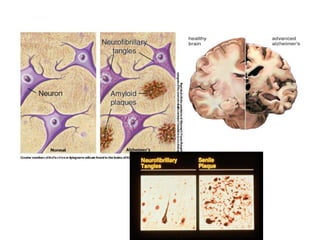
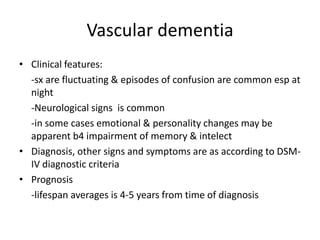
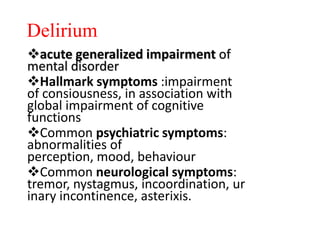
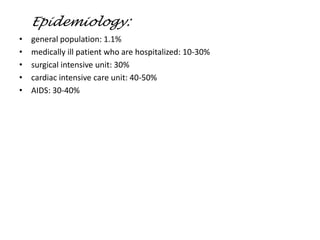
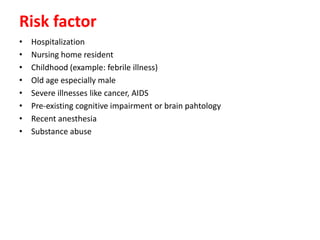
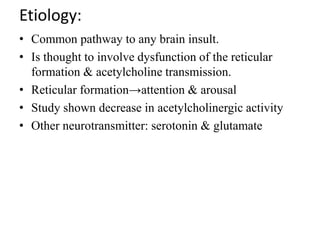
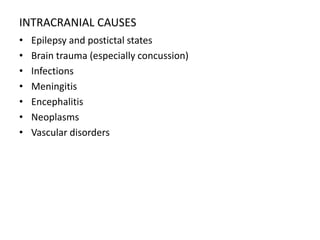
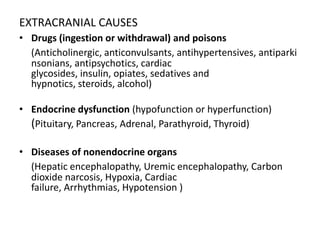
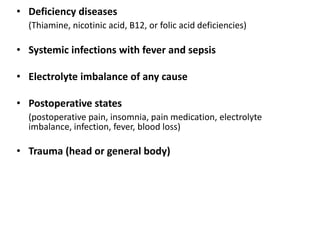
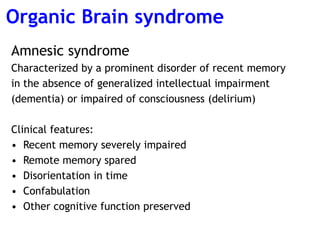
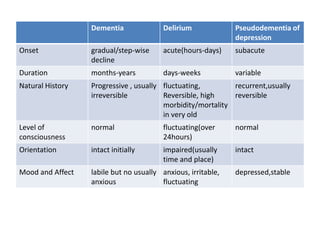
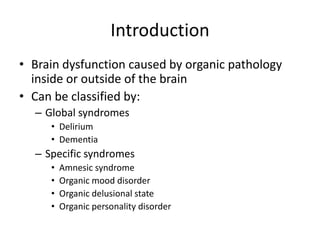
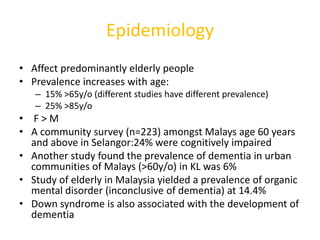
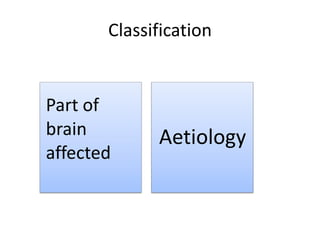
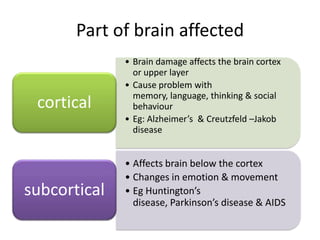
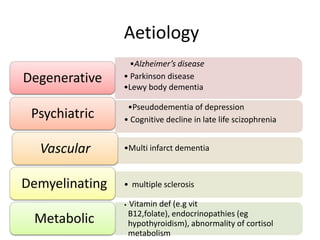
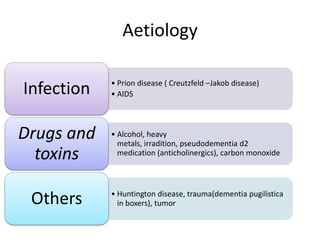
This document provides information on organic brain syndrome, including dementia and delirium. It defines organic brain syndrome as brain dysfunction caused by pathology inside or outside the brain. Dementia is described as the acquired impairment of cognitive functions such as memory and orientation, while delirium is an acute impairment of consciousness and cognition. The document discusses the epidemiology, risk factors, pathologies, clinical features, investigations, and management of various types of organic brain syndrome including Alzheimer's disease and vascular dementia.
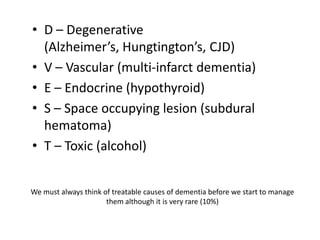
![VITAMIN D VEST
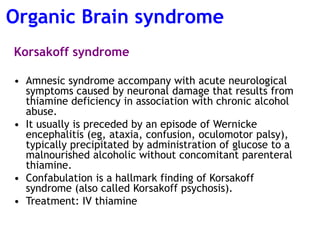
• V – Vitamin Deficiency [B12, folate and
thiamine(Wernicke-korsakoff)]
• I – Intracranial masses (tumour, abscess)
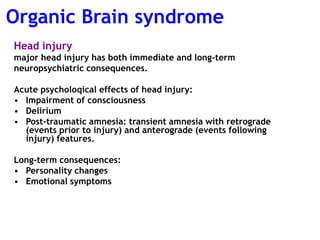
• T – Trauma (head injury, dementia pugilistica)
• A – Anoxia
• M- Metabolic (diabetes)
• I – Infection (HIV, syphilis, Creutzfeldt-Jakod)
• N- Normal pressure hydrocephalus](https://image.slidesharecdn.com/organicbrainsyndrome-130619180626-phpapp02/85/Organic-brain-syndrome-9-320.jpg)