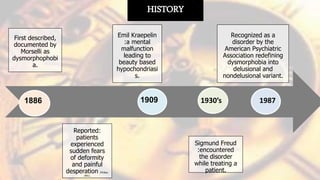
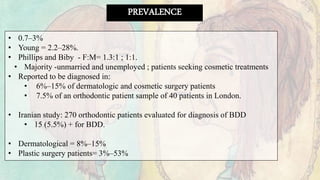
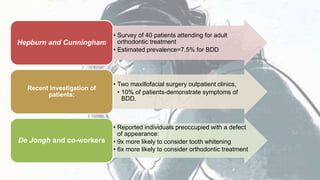
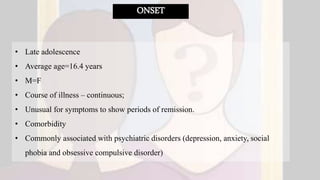
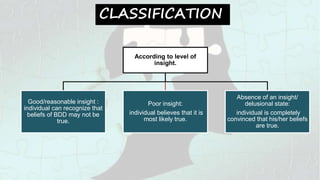
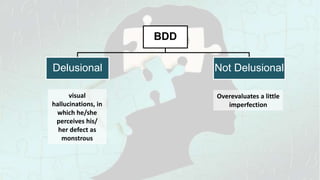
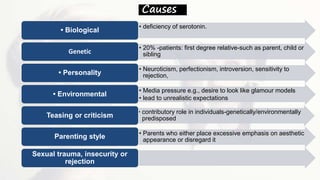
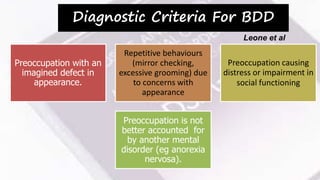
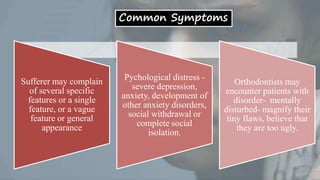
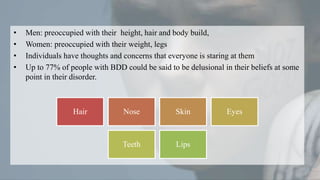
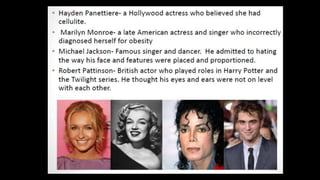
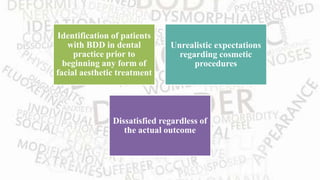
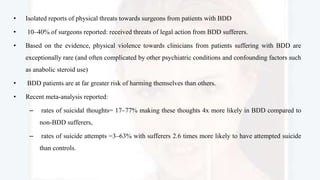
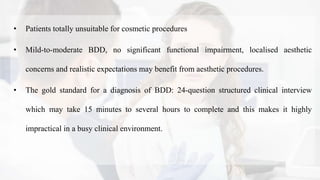
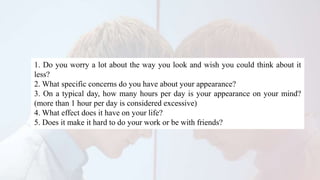
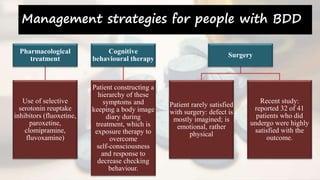
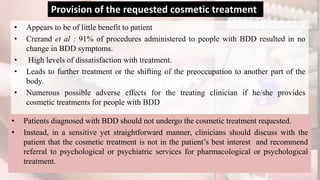
Body dysmorphic disorder (BDD) is a psychological disorder where patients are excessively concerned about a perceived flaw in their physical appearance. BDD was first described in the late 19th century and is now recognized by the American Psychiatric Association. It affects about 0.7-3% of the population and commonly presents in dental practices. Patients with BDD may request cosmetic procedures but are rarely satisfied with treatment outcomes and their concerns typically shift to another body part. The disorder is best managed through cognitive behavioral therapy and medication rather than further cosmetic treatments.