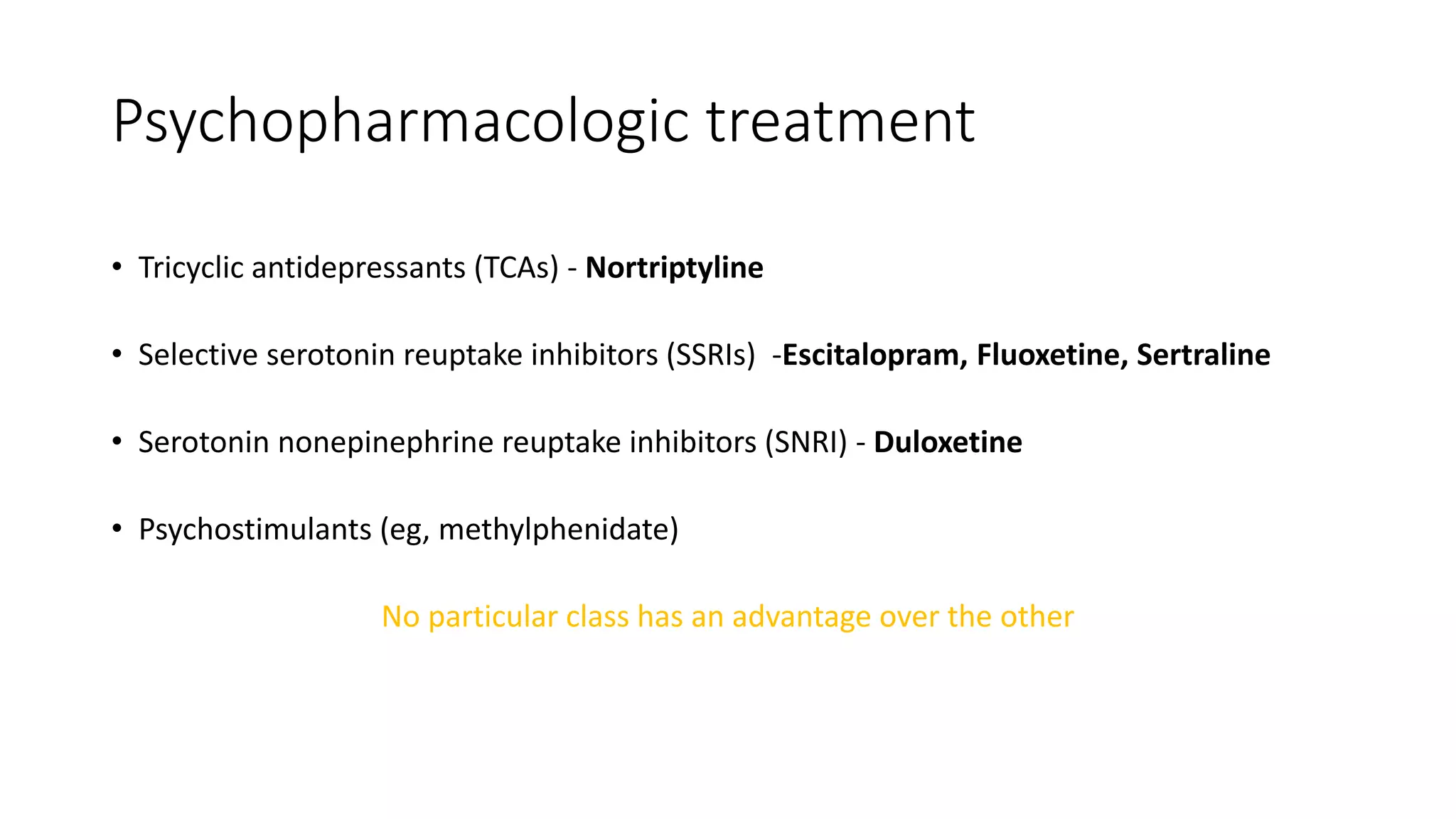
This document summarizes various neuropsychiatric sequelae that can occur after a stroke. It discusses conditions like post-stroke depression (occurring in 30-40% of patients), anxiety disorders (25%), apathy (20%), pathological laughing/crying (11-35%), catastrophic reactions (20%), and more rare conditions like mania, bipolar disorder, and psychosis. It provides details on risk factors, pathophysiology, diagnosis, and treatment approaches for these different post-stroke neuropsychiatric conditions.