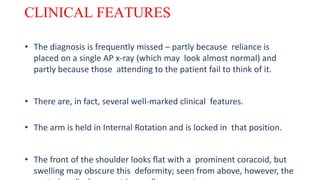
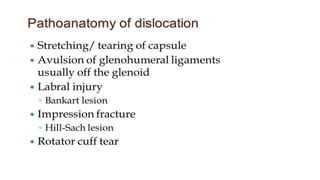
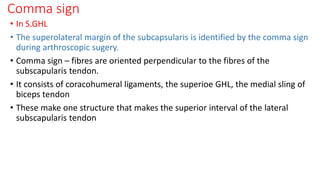
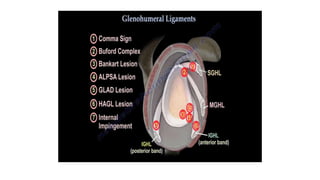
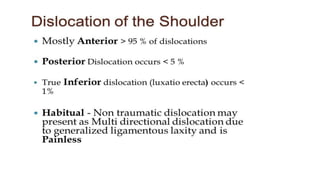
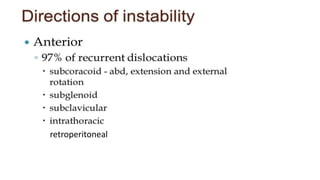
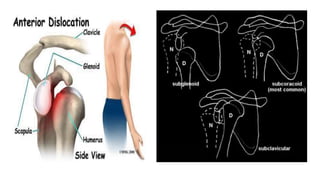
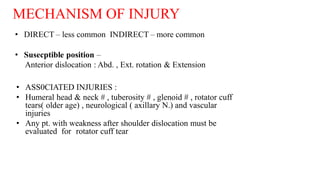
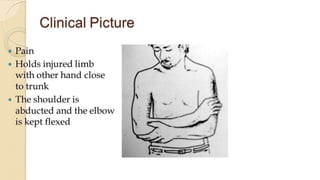
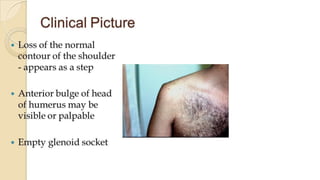
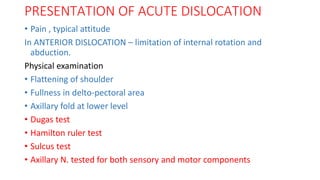
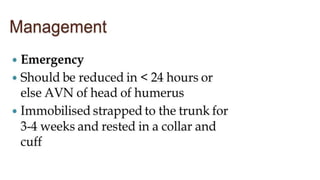
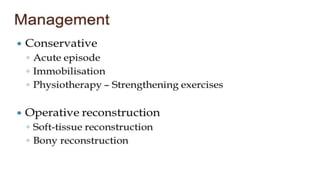
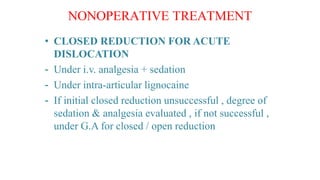
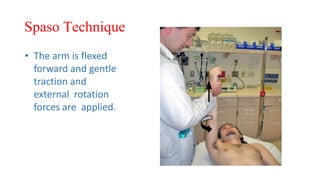
The document discusses shoulder joint instability, detailing the anatomy, common injuries, and classification systems related to dislocations and lesions of the shoulder. Various surgical and non-surgical treatment options, including specific techniques for acute dislocation and recurrent instability, are explored. It emphasizes the importance of proper diagnosis, evaluation methods, and rehabilitation strategies for effective management of shoulder instability.

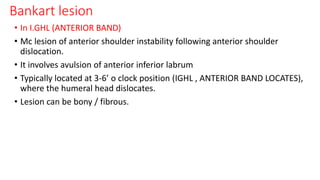
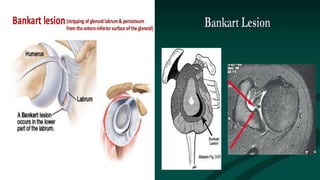
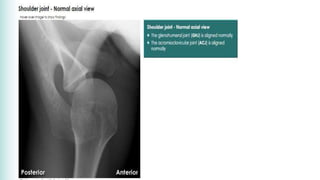
![• Most mobile joint in the body
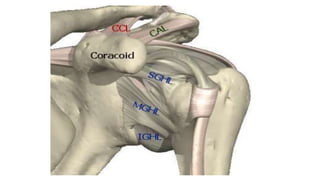
• Synovial joint….. Ball and socket joint
• Articular surfaces- head of the humerus + glenoid cavity
both covered by hyaline cartilage.
• Size of head of humerus is 3-4 times larger than the glenoid cavity.
[ glenoid labrum (lip) covers excess part of the head ]- fibrocartilaginous rim
Labrum Increases humeral contact to 75%
• Adv- increased shoulder ROM
• Disadv – stability of the joint decreases.](https://image.slidesharecdn.com/shoulderjointinstability-190822062137/85/Shoulder-joint-instability-2-320.jpg)




![BANKART OPERATION alone 67% recurrence rate.
• Remplissage (French-”to fill in”) procedure done for Hill sachs lesion
which involves >30% of articular surface.
• Infraspinatous tendon inserted into Hill sachs lesion.
• [Bankart surgery + Remplissage]- 10% recurrence rate.
• complications
• Excessive tightening of ant. Capsule and subscapularis can restrict ext. rotations
and functions and may cause degenerative joint disease known as
capsulorrhaphy arthropathy.](https://image.slidesharecdn.com/shoulderjointinstability-190822062137/85/Shoulder-joint-instability-57-320.jpg)