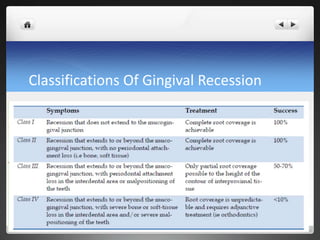
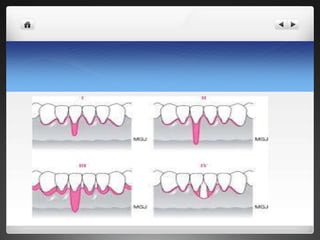
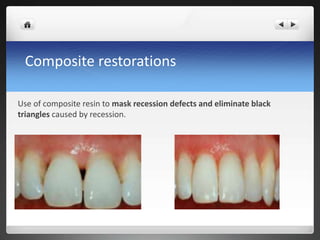
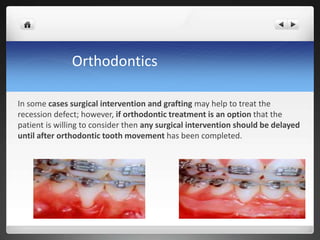
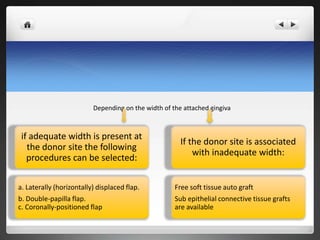
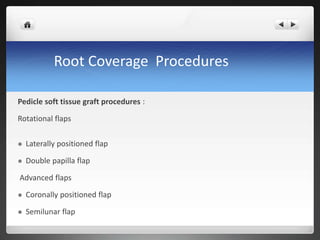
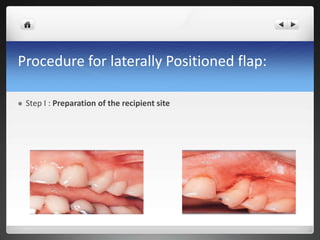
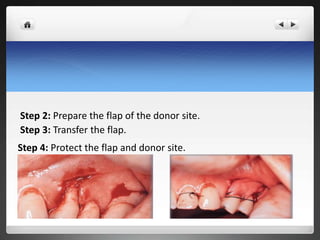
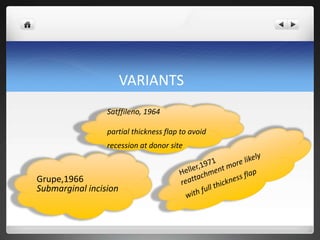
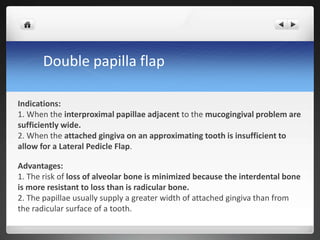
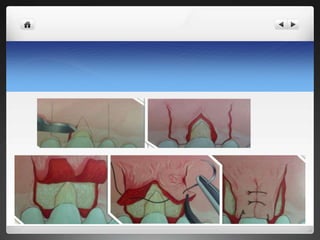
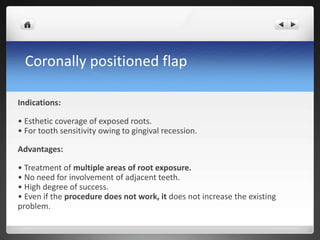
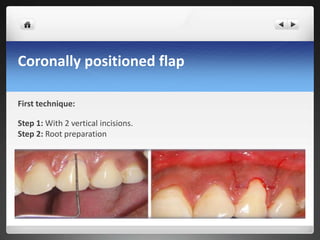
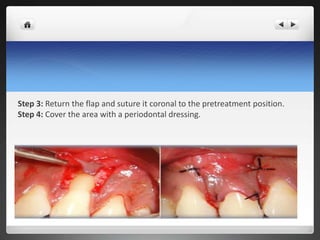
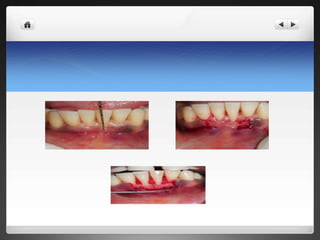
This document discusses various root coverage procedures for treating gingival recession. It begins by defining gingival recession and classifying types. Nonsurgical treatments including monitoring, desensitizing agents, and restorations are outlined. Surgical options such as laterally positioned flaps, double papilla flaps, coronally positioned flaps, free gingival grafts, and subepithelial connective tissue grafts are described in detail. Factors in selecting a procedure and modifications to techniques are also summarized. The document concludes that careful case selection and surgical management are key to achieving successful root coverage outcomes.

![Definition
GINGIVAL RECESSION-
Gingival recession is defined as the
apical migration of the junctional epithelium
with exposure of root surfaces. [Kassab MM, Cohen RE-2003].
Gingival recession is the apical shift
of the marginal gingiva from
its normal position on the
crown of the tooth to levels on the root surface beyond the
cemento enamel junction [Loe H-1992].](https://image.slidesharecdn.com/seminar6-171217094744/85/ROOT-COVERAGE-PROCEDURES-3-320.jpg)