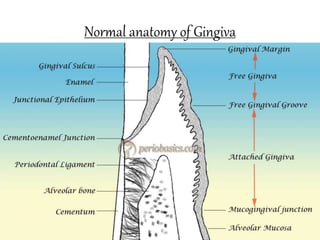
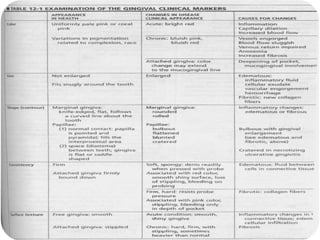
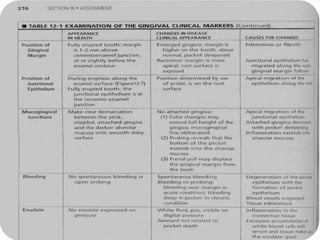
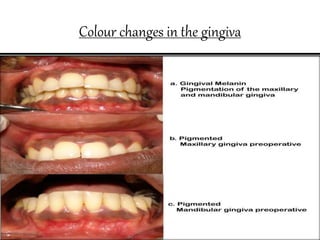
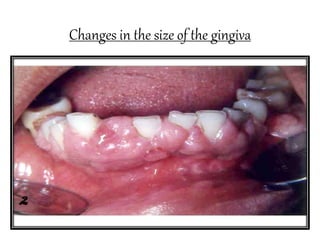
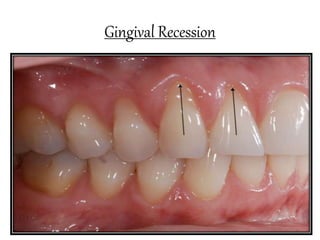
This document discusses the clinical features of gingivitis. It begins by defining gingivitis as inflammation of the gingiva and describes how plaque bacteria can damage gingival tissues. It then covers the different types of gingivitis based on duration and distribution. Key signs of gingivitis that are discussed include gingival bleeding, color changes, changes in consistency, size, surface texture, position and contour. Specific conditions like gingival recession are also explained in terms of definition, classification, etiology and clinical significance.