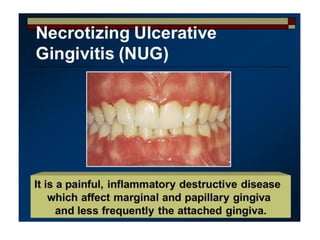
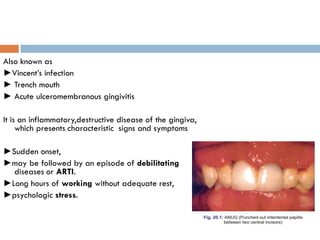
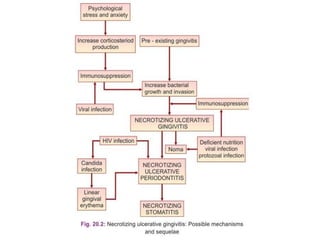
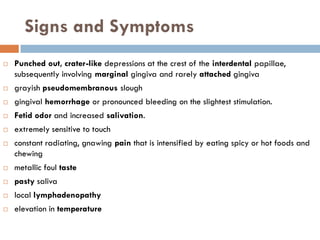
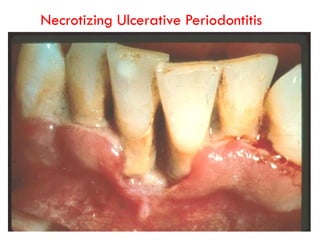
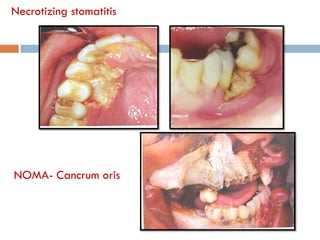
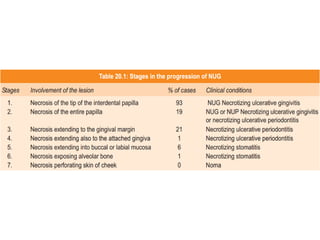
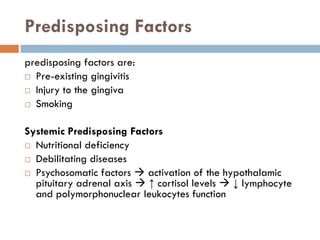
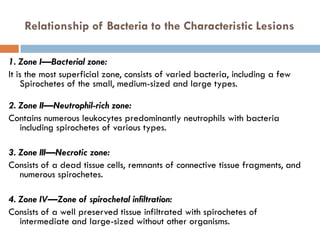
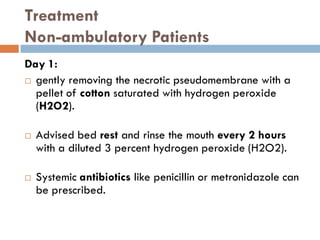
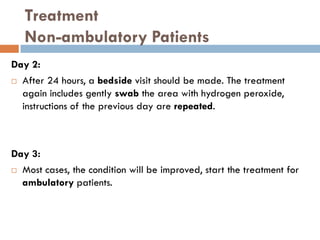
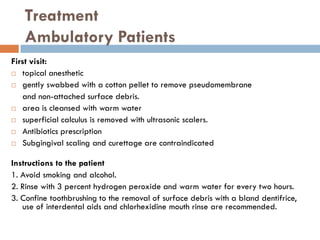
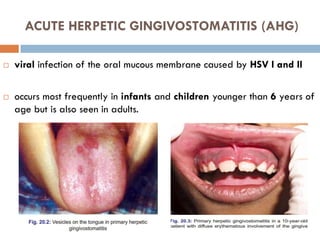
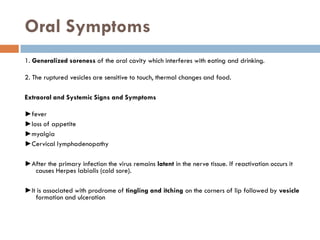
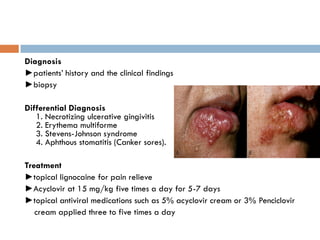
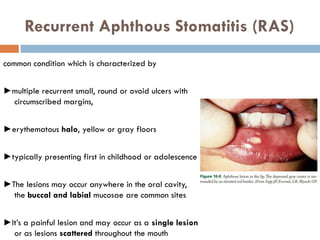
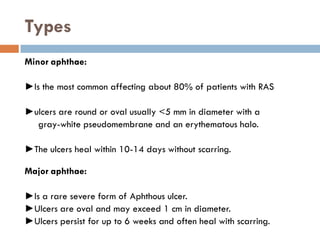
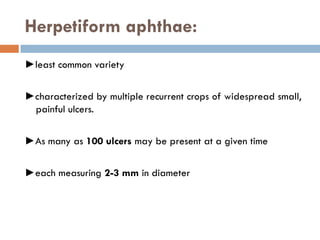
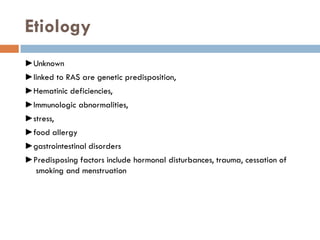
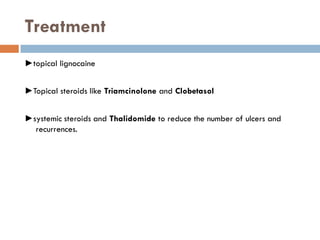
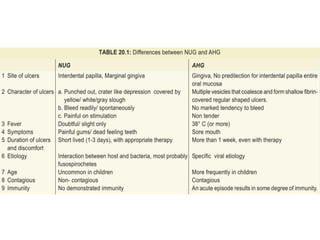
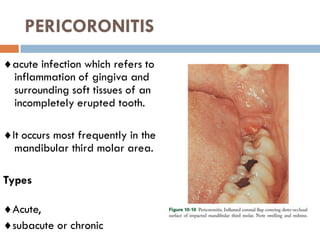
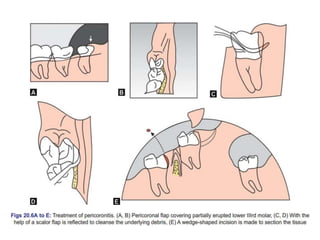
This document discusses and classifies various acute gingival infections including traumatic lesions, viral infections like herpetic gingivostomatitis, bacterial infections like necrotizing ulcerative gingivitis, fungal diseases, gingival abscesses, aphthous ulcers, erythema multiforme, and drug allergies. It provides detailed information on necrotizing ulcerative gingivitis including causes, signs and symptoms, stages, predisposing factors, relationship to bacteria, and treatment approaches. It also summarizes acute herpetic gingivostomatitis, recurrent aphthous stomatitis, and pericoronitis covering causes, clinical features, types