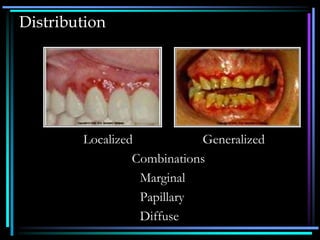
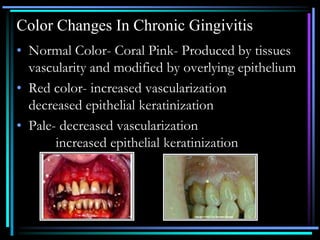
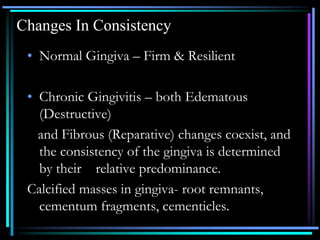
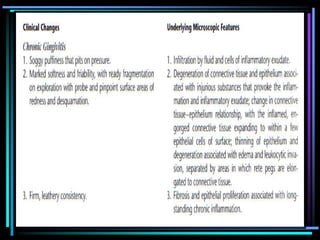
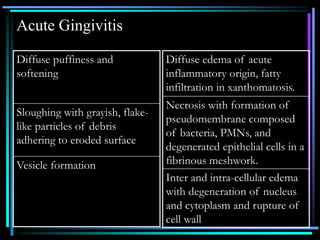
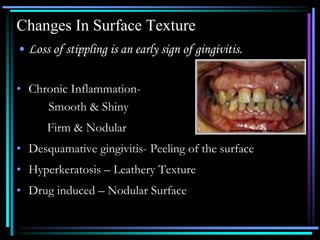
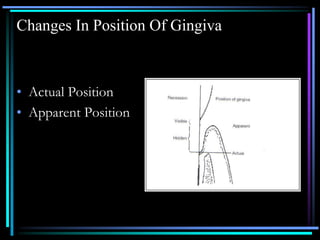
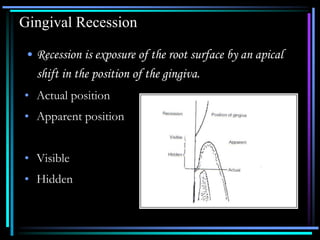
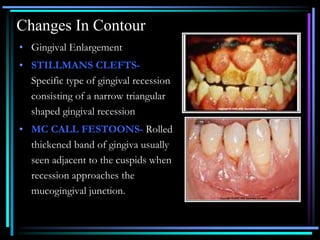
This document summarizes the clinical features of gingivitis. It describes the different types of gingivitis including acute, chronic, and recurrent gingivitis. It discusses the distribution, clinical findings such as bleeding and color changes, and causes of gingivitis. Local factors like trauma from toothbrushing and systemic factors like vitamin deficiencies that can cause abnormal bleeding are explained. The document also covers changes in gingival consistency, position, contour and other signs of gingivitis.