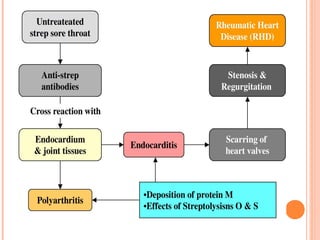
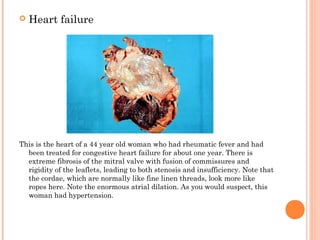
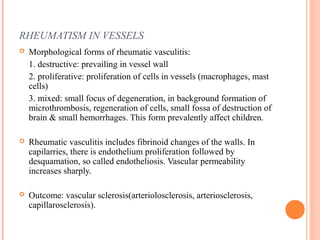
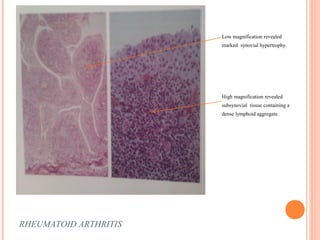
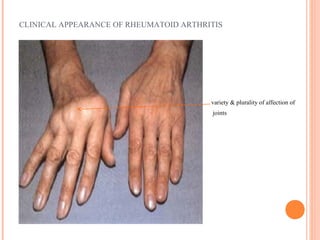
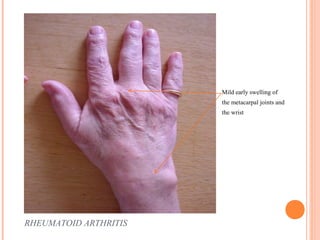
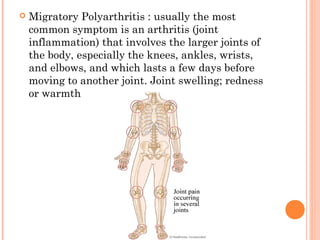
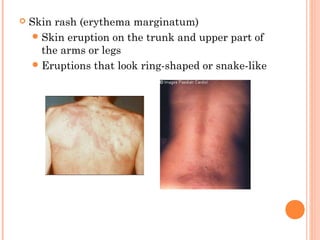
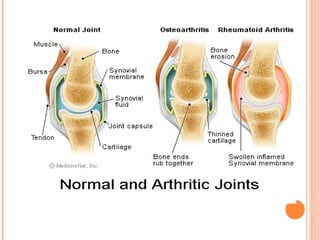
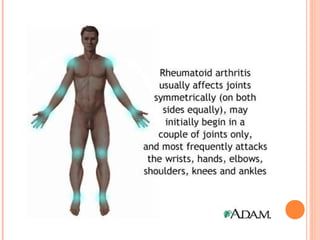
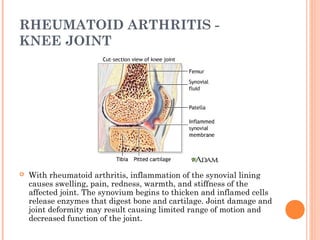
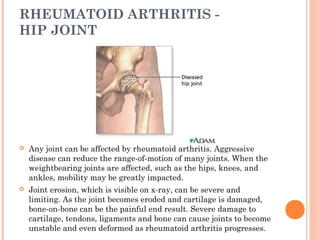
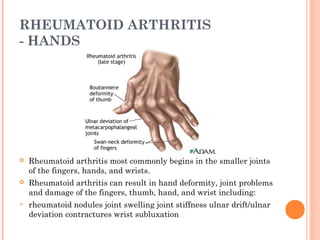
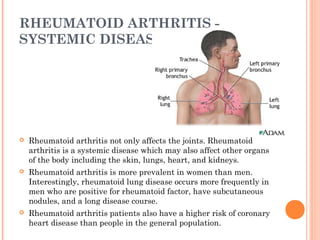
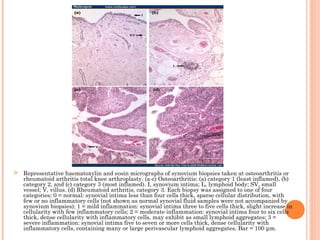
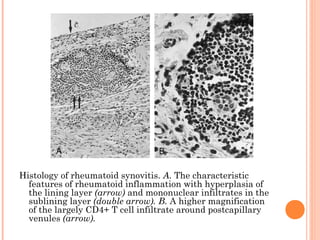
Rheumatic fever is an inflammatory disease that can affect the heart, joints, nervous system and skin following a streptococcus infection such as strep throat. It primarily affects children aged 5 to 15 years old. Rheumatoid arthritis is an autoimmune disease where the immune system attacks the body's own tissues, causing chronic inflammation of the joints and surrounding tissues. It can also affect other organs and is considered a systemic illness. Both conditions involve inflammation and can damage tissues over time.