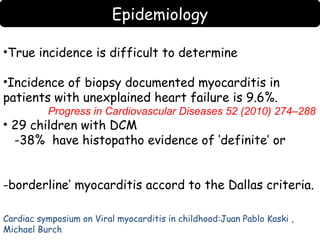
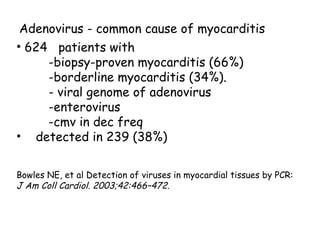
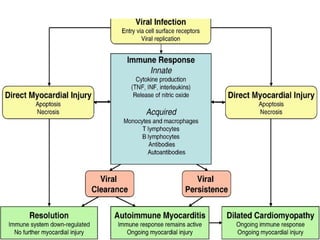
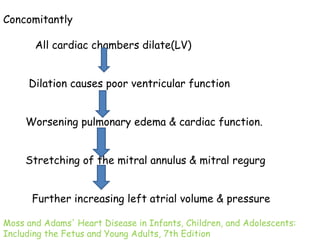
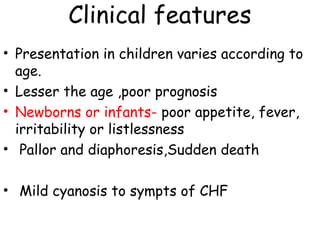
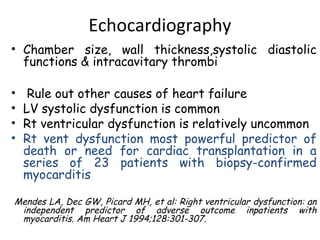
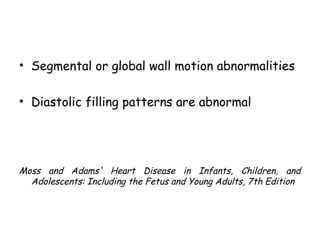
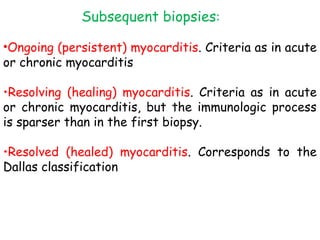
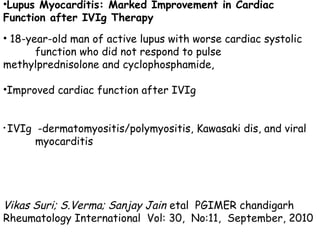
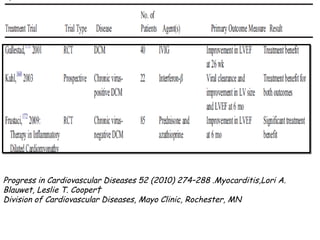
This document discusses myocarditis in children. It defines myocarditis and describes the epidemiology, etiology, pathophysiology, clinical presentation, diagnosis and treatment. Myocarditis has many potential causes including viruses like adenovirus and enterovirus. Clinically it presents variably depending on age from nonspecific symptoms to heart failure. Diagnosis involves blood tests, ECG, imaging like echocardiogram and cardiac MRI, and endomyocardial biopsy. Treatment is supportive with heart failure medications, antivirals may help, and immunosuppressants can reduce inflammation and improve function.