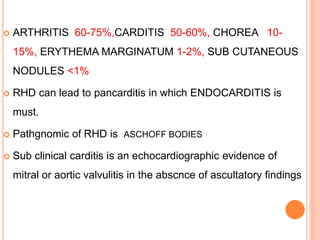
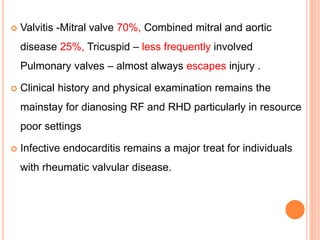
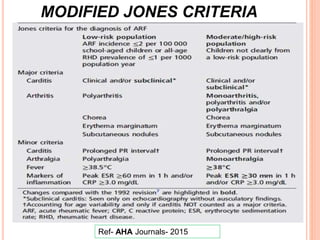
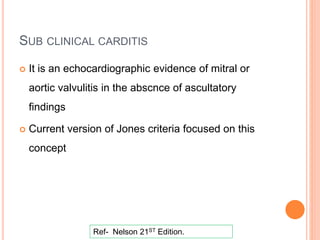
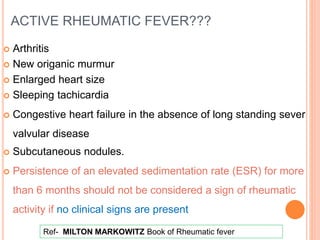
Rheumatic heart disease is a major complication of rheumatic fever, triggered by group A streptococcal throat infections, leading to inflammation of the heart and potential valve damage. It primarily affects children in developing nations and is characterized by symptoms such as carditis, polyarthritis, and chorea, with significant laboratory findings including elevated inflammatory markers and echocardiographic evidence of heart involvement. Long-term effects include severe valvular diseases, particularly affecting the mitral valve, which can result in heart failure and other serious complications.
![RHEUMATIC FEVER – [ Rheumatic – Joints]
Rheumatic fever is an acute, immunologically mediated
multisystemic inflammatory disease that follows group A beta
haemolytic streptococcus infection of the throat.
“Licks the JOINT, bites the HEART”
- Lasegue](https://image.slidesharecdn.com/rhdpresentation-240725173950-613ee210/85/RHD-presentation-pptx-2-320.jpg)



![GROUP A BETA HEMOLYTIC STREPTOCOCCI
Gram-positive coccoid shaped bacteria grows in chains.
Broadly classified by their hemolytic activity
Beta hemolytic -
SEQUELA M TYPE
ACUTE RHEUMATIC FEVER 1, 3, 5, 6, 18, 29 [ pharyngeal
serotypes]
ACUTE GLOMERULONEPHRITIS
Throat 1, 4, 12
Skin 49, 55, 57, 60.
Ref- Nelson 21ST Edition.](https://image.slidesharecdn.com/rhdpresentation-240725173950-613ee210/85/RHD-presentation-pptx-6-320.jpg)




















![CHRONIC SEVERE INSUFFIENCY
Leaflet and chordal thickening, chordal fussion and restricted
leaflet motion secondary to fibrosis
Persistent mitral insuffiency
Increased Pulmonary artery pressure[PAH]
Development of RA/RV dilatation
RIGHT HEART FAILURE](https://image.slidesharecdn.com/rhdpresentation-240725173950-613ee210/85/RHD-presentation-pptx-35-320.jpg)

























![Mitral Valve Prolapse [floppy mitral valve, click
syndrome, or Barlow's syndrome ]
• Benign disorder
• It can be distinguished from its rheumatic counterpart
clinically on the basis of the characteristic systolic click and
late systolic murmur.
• Echocardiography is the most reliable way to confirm the
diagnosis.](https://image.slidesharecdn.com/rhdpresentation-240725173950-613ee210/85/RHD-presentation-pptx-63-320.jpg)












![POINTS TO REMEMBERED...
Rheumatic fever is an acute, immunologically mediated
multisystemic inflammatory disease that follows group A beta
haemolytic streptococcus { 1, 3, 5, 6, 18, 29 [ pharyngeal
serotypes]} infection of the throat.
In India incidence of rheumatic fever by eco studies is 0.5 to 11
per thousand, most common age group is 5-15
Diagnosis is based on MODIFIED JONES CRITERIA
Exceptions for Jones criteria is Carditis, recurrence of
Rheumatic fever and Choria.](https://image.slidesharecdn.com/rhdpresentation-240725173950-613ee210/85/RHD-presentation-pptx-79-320.jpg)