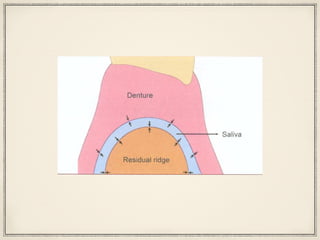
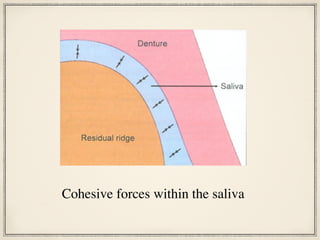
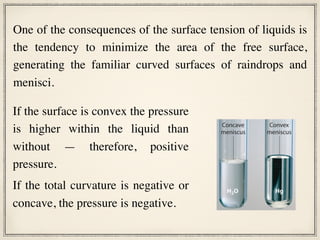
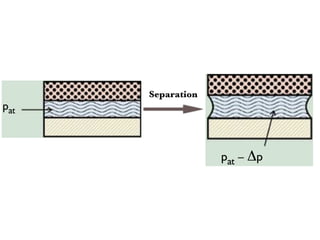
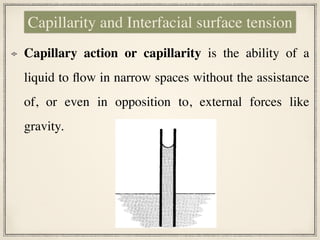
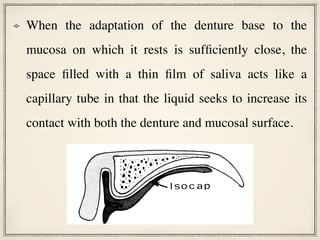
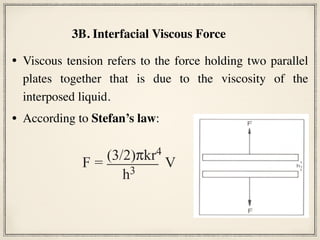
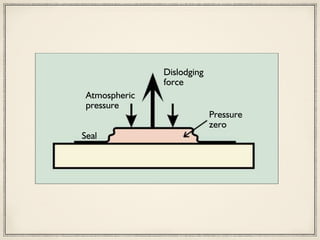
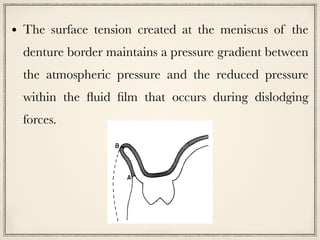
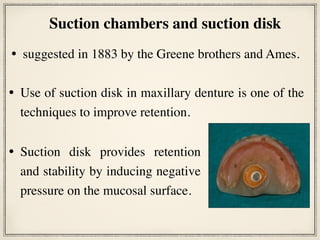
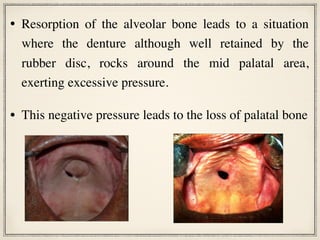
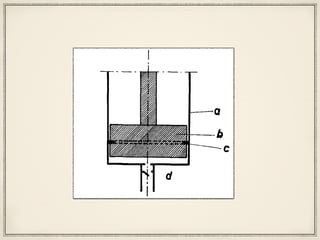
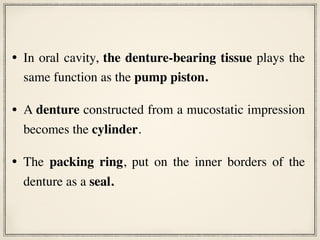
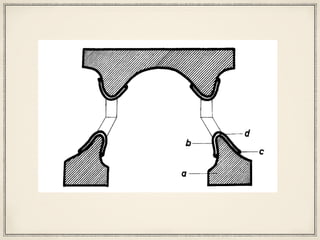
The document discusses factors that affect retention of complete dentures. It identifies physical factors like adhesion, cohesion, interfacial forces, gravity, and atmospheric pressure. It also discusses biological factors like intimate tissue contact and border seal, and mechanical factors like undercuts and suction chambers. Interfacial surface tension and viscous tension contribute to interfacial forces. Maximizing surface area, minimizing space between denture and tissue, and increasing fluid viscosity can improve denture retention based on these physical principles. However, atmospheric pressure alone does not provide static retention without a vacuum seal being present.