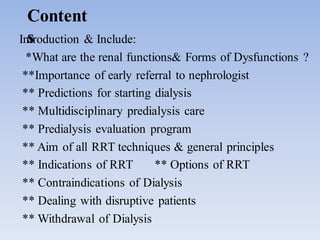
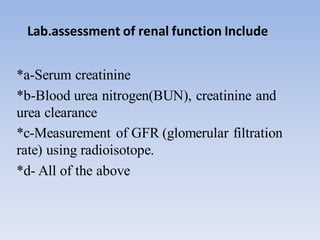
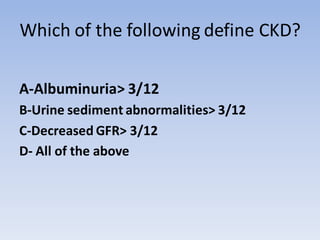
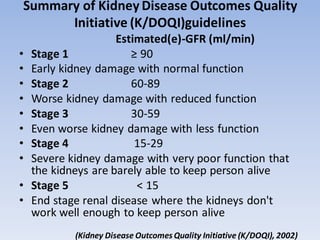
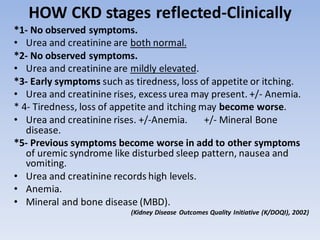
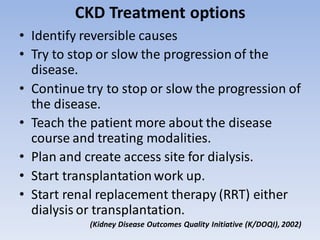
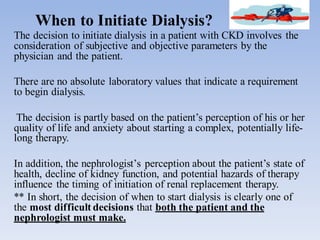
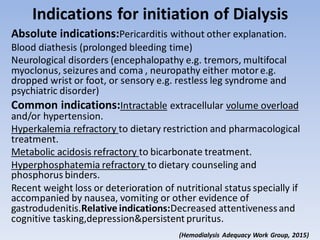
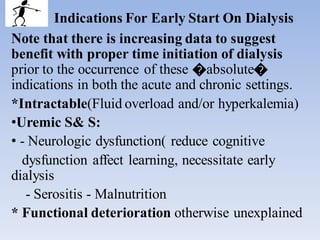
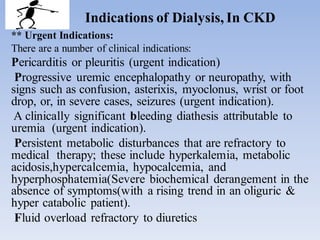
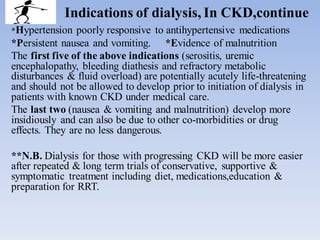
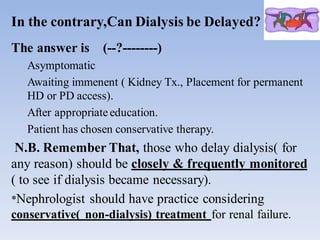
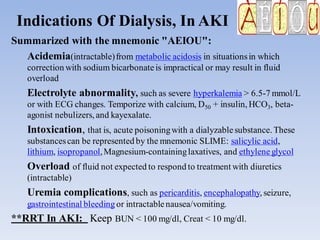
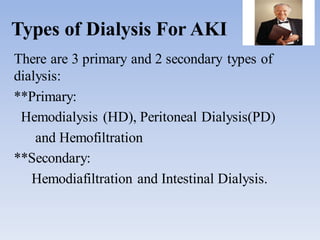
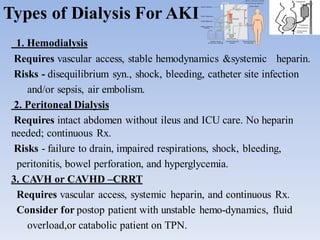
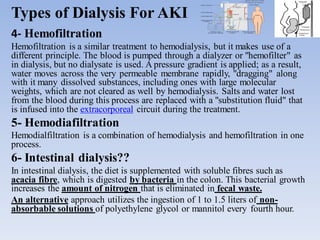
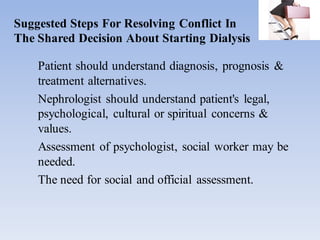
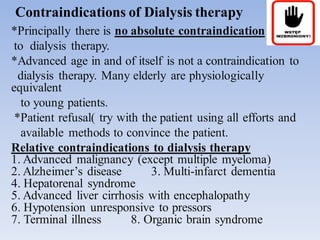
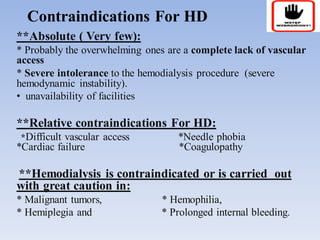
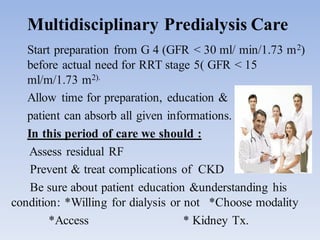
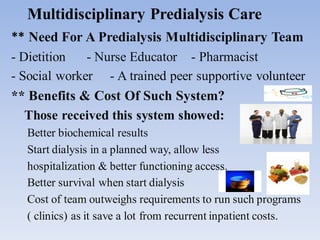
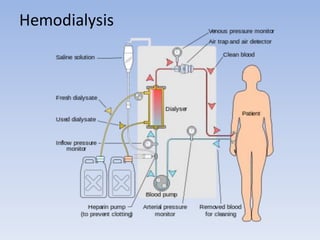
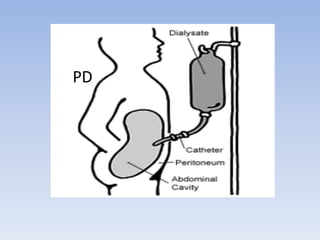
The document discusses renal replacement therapy (RRT) and indications for dialysis. It provides definitions of dialysis and notes it is used for acute kidney injury (AKI) and end-stage renal disease (CKD stage 5). For AKI, the main indications for dialysis are electrolyte abnormalities, fluid overload, and uremia complications. Hemodialysis, peritoneal dialysis and hemofiltration are the primary RRT modalities for AKI. For CKD, indications include refractory fluid overload, metabolic abnormalities, and symptoms like nausea/vomiting or malnutrition. The decision to start dialysis involves clinical status and quality of life considerations.