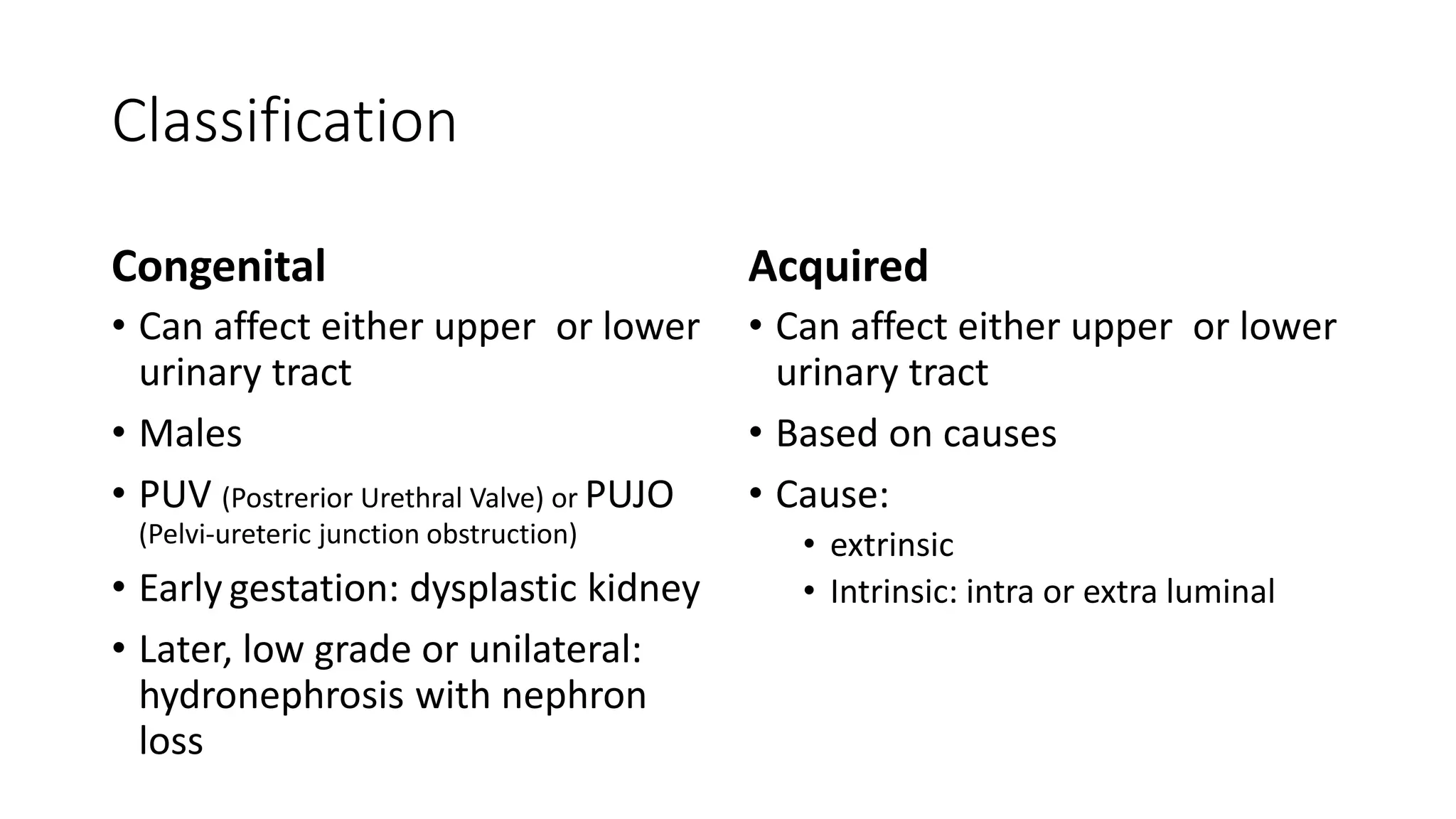
This document discusses renal stones and obstructive uropathy. It covers the etiology and pathogenesis of renal stones, including idiopathic calcium urolithiasis, hypercalcemic disorders, renal tubular syndromes, uric acid lithiasis, and enzyme disorders. It also discusses clinical features, complications, stone management approaches like ESWL, ureteroscopy, and PCNL, and medical treatment options. Regarding obstructive uropathy, it defines key terms, discusses classifications like congenital and acquired causes, clinical features, imaging approaches, and treatment indications and options like nephrectomy, pyeloplasty, and endoscopic procedures.