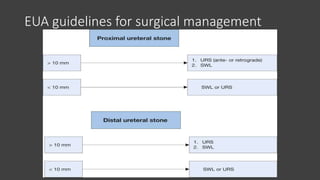
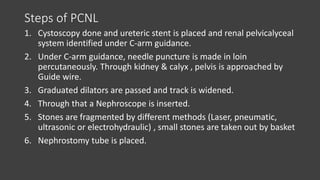
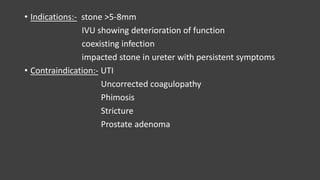
This document provides an overview of renal stones (nephrolithiasis). It discusses the anatomy of the kidneys, types of stones, risk factors and pathophysiology. Symptoms include flank pain and hematuria. Diagnosis is typically made using non-contrast CT. Treatment depends on stone size and location, and may include conservative management, extracorporeal shock wave lithotripsy (ESWL), percutaneous nephrolithotomy (PCNL), or ureteroscopic stone removal (URS). Surgical procedures aim to break up or remove stones to allow passage. Complications can include bleeding, infection, and injury to surrounding structures.