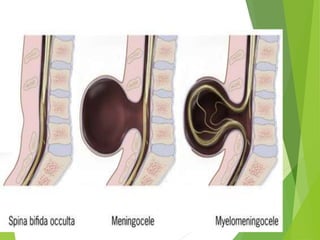
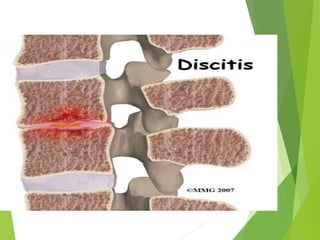
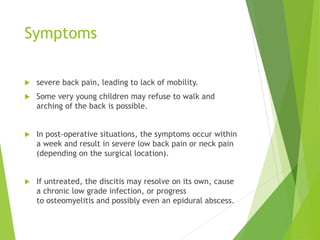
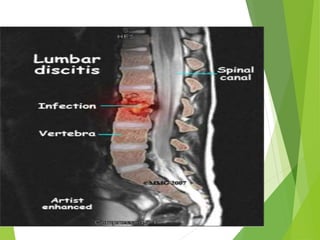
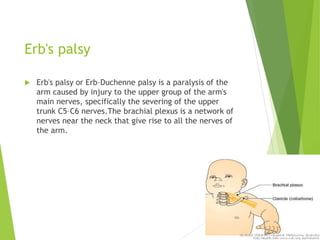
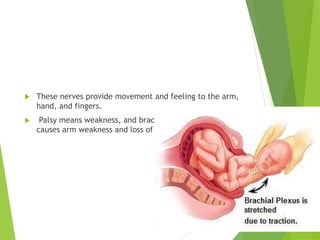
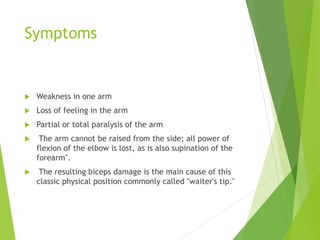
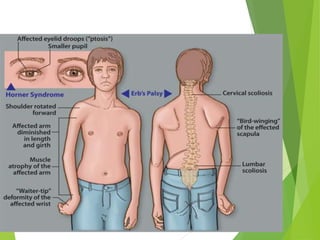
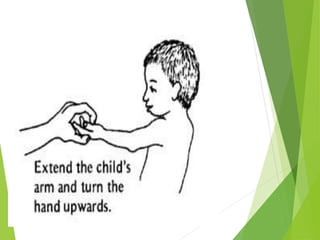
Myelomeningocele is a type of spina bifida where the backbone and spinal canal do not fully close before birth, resulting in a sac-like protrusion of the spinal cord and meninges through the defect. It is the most common and severe type of spina bifida and can cause paralysis, loss of bladder/bowel control, and other neurological issues. Discitis is an infection of the intervertebral disc that causes severe back pain and lack of mobility. Erb's palsy is paralysis of the arm caused by injury to the brachial plexus nerves during difficult childbirth, resulting in weakness and loss of movement in the arm.