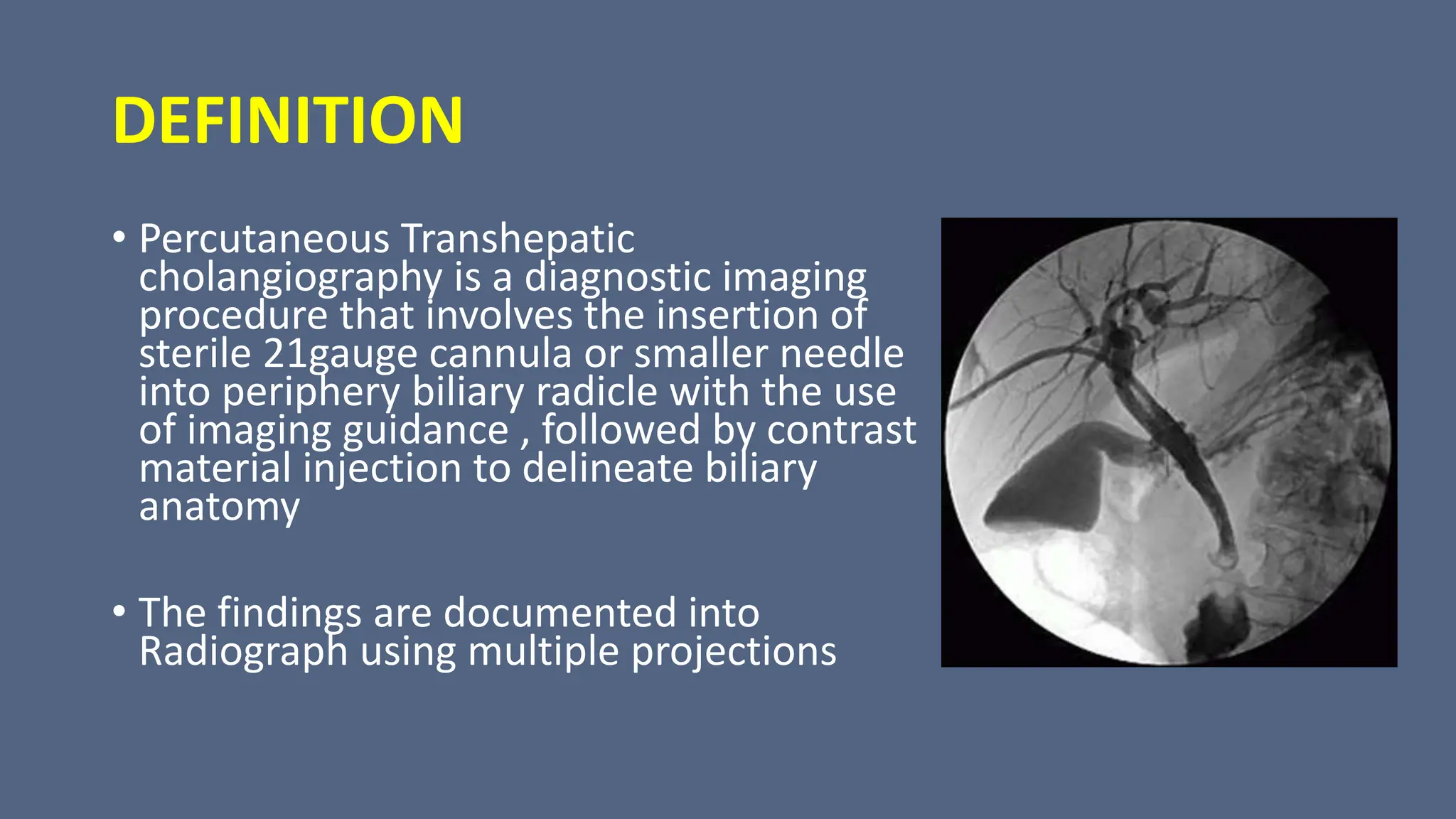
The document provides a comprehensive overview of percutaneous transhepatic cholangiography (PTC) and percutaneous transhepatic biliary drainage (PTBD), detailing the definitions, indications, contraindications, preparation, techniques used, and potential complications associated with these procedures. It covers methods of imaging the biliary tract, essential equipment, and the procedural steps involved in navigating biliary obstruction. The document emphasizes the significance of pre-procedural imaging and patient monitoring to ensure effective management and mitigate risks during and after the interventions.