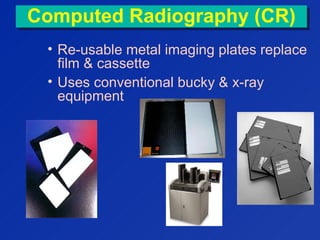
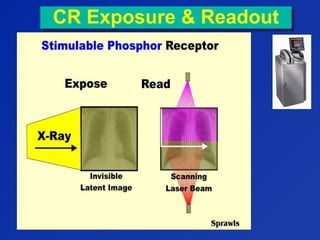
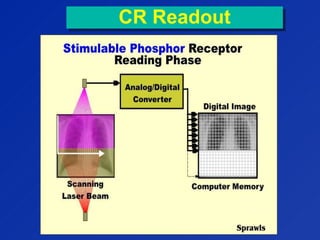
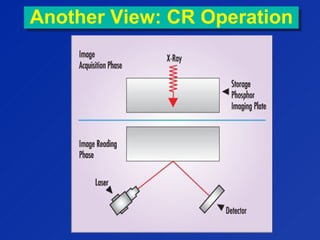
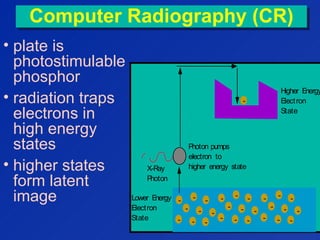
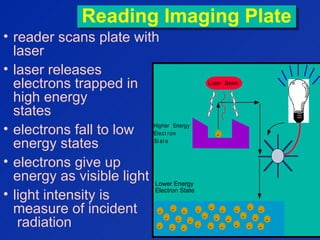
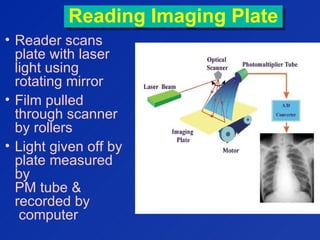
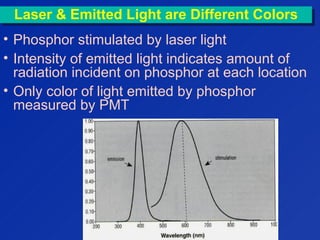
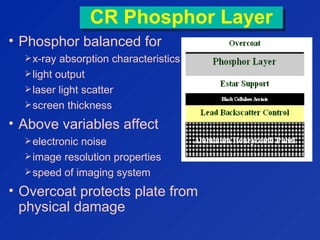
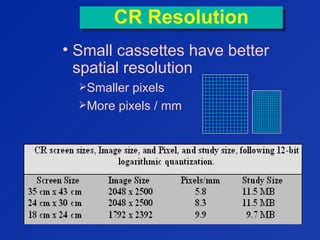
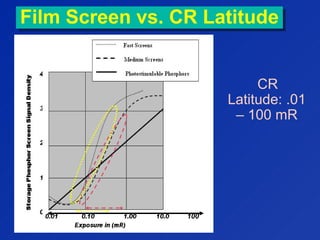
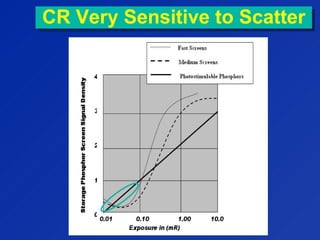
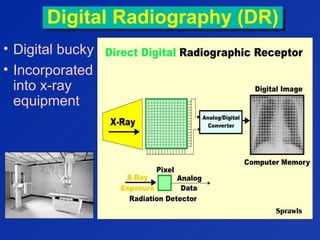
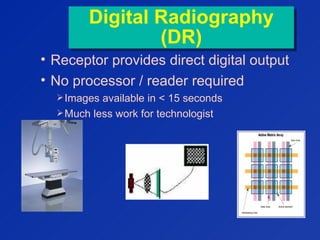
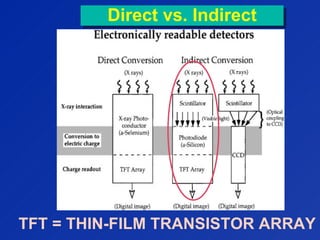
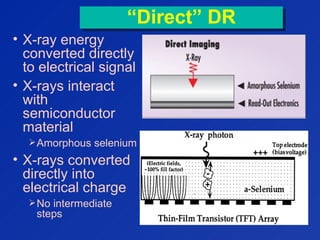
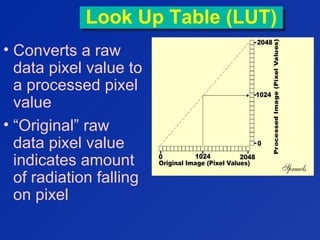
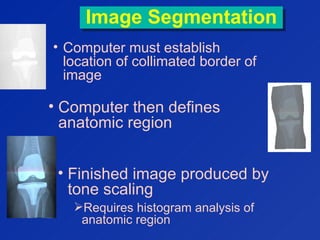
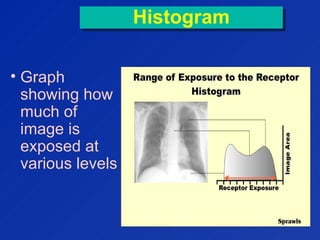
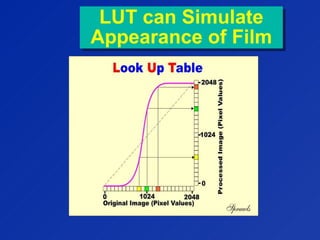
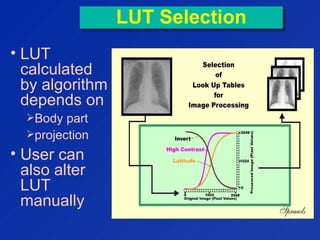
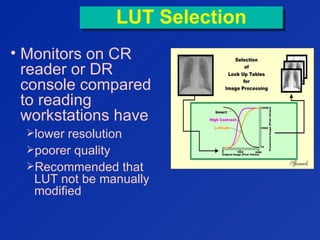
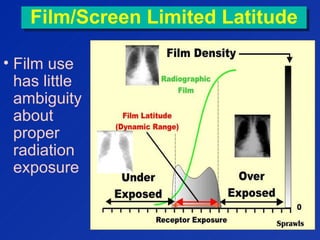
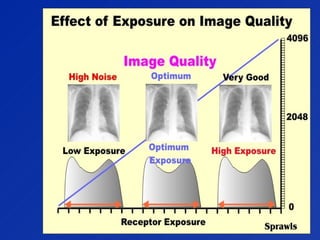
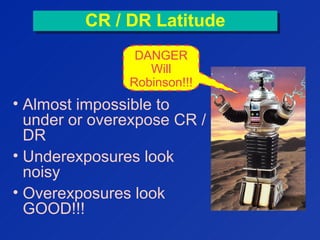
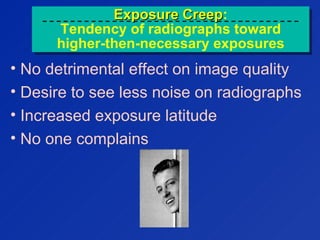
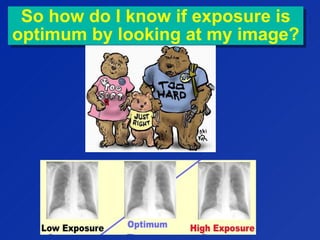
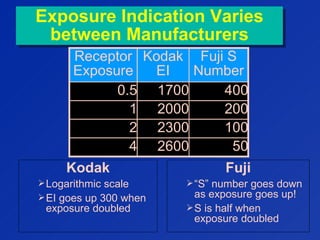
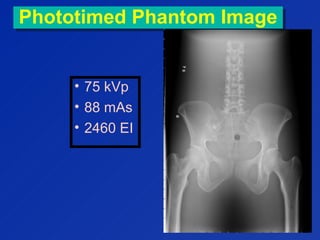
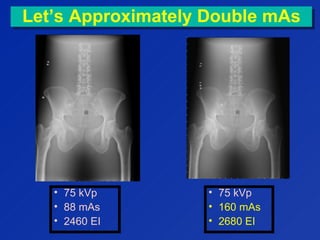
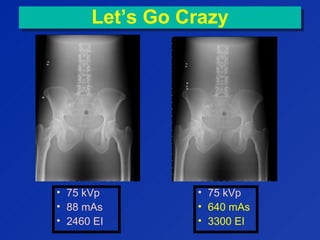
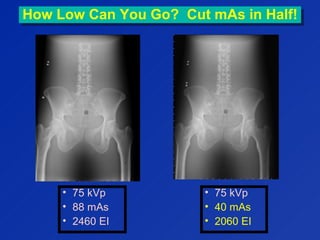
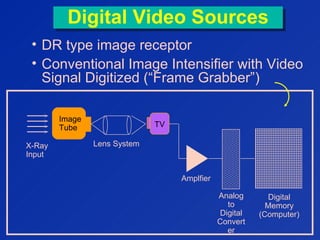
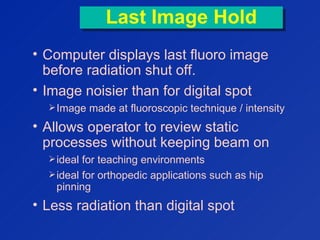
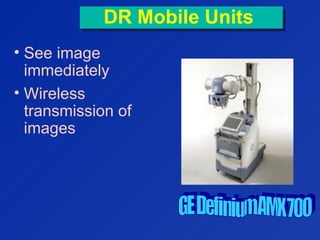
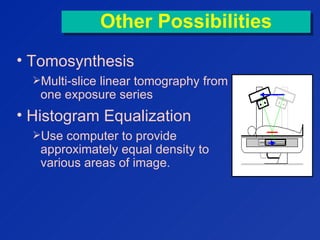
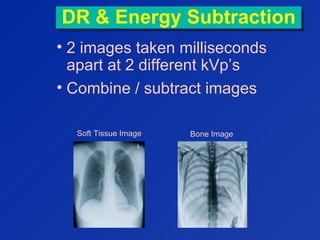
This document discusses computed radiography (CR) and digital radiography (DR). CR uses reusable imaging plates instead of film, which are read by a laser scanner. DR uses a digital detector incorporated into x-ray equipment to provide direct digital output. Both have greater exposure latitude than screen-film and allow computer post-processing to enhance images. Technologists must monitor exposure indices to avoid overexposure with CR and DR systems. The document also covers digital fluoroscopy techniques like frame averaging.