This document provides an overview of meningitis including:
- It is an inflammation of the meninges that can be caused by bacteria, viruses, fungi or tuberculosis. Common bacterial causes are Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae type b.
- An outbreak in Nigeria from 2016-2017 saw over 1,400 suspected cases mostly in children ages 5-14 in certain states. Risk factors include young age, close contacts, crowding and poverty.
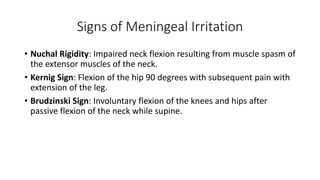
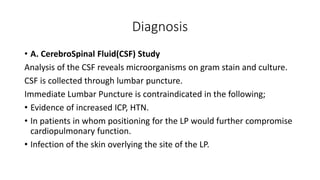
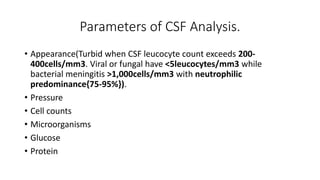
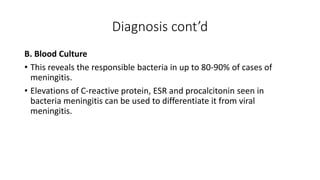
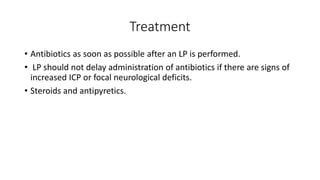
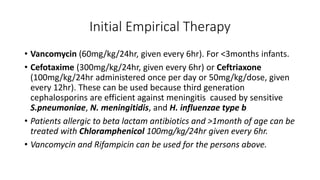
- Symptoms can include fever, headache, nausea, and signs of meningeal irritation like neck stiffness. Diagnosis involves CSF and blood tests. Treatment depends on the suspected cause but may include