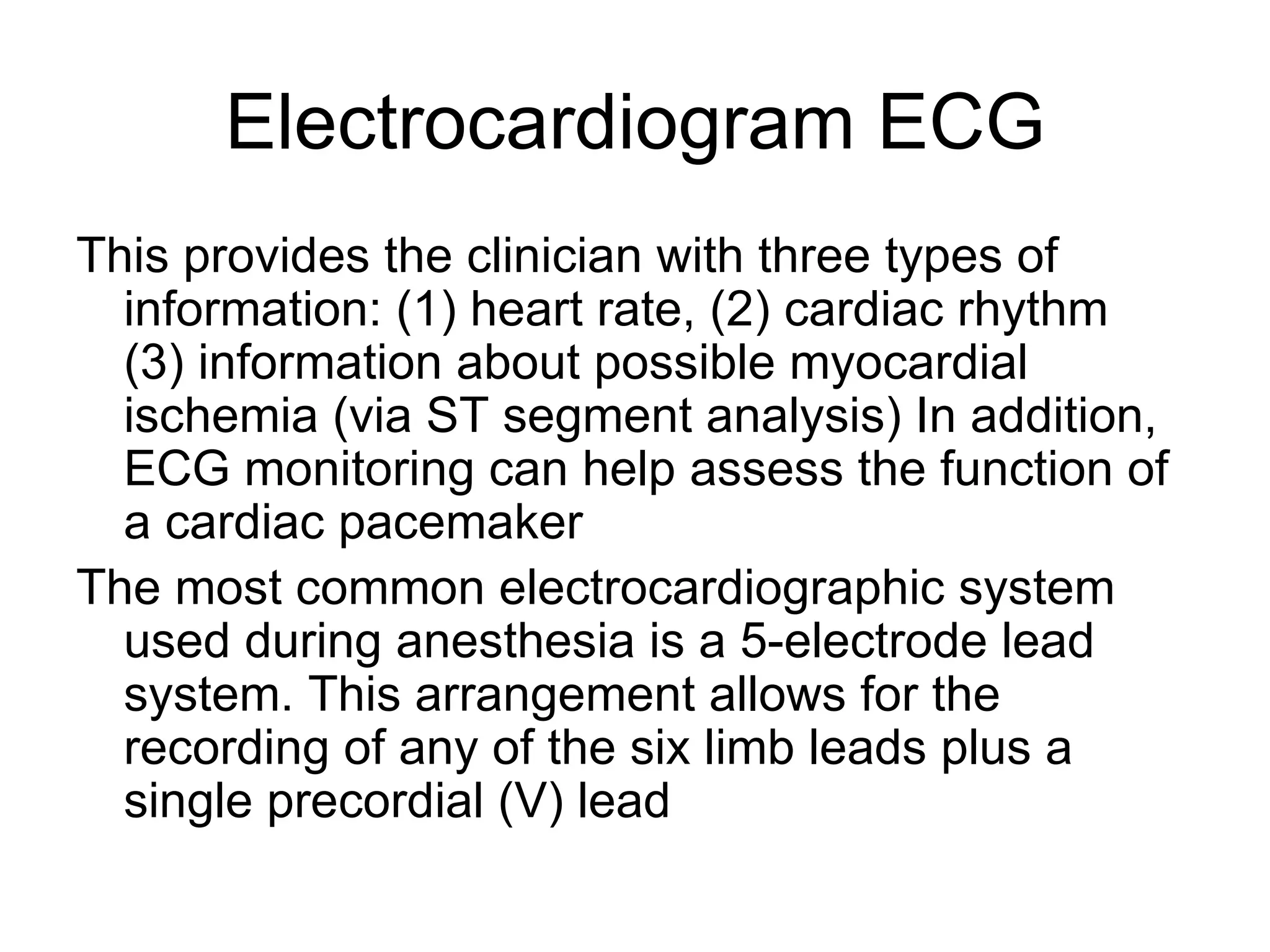
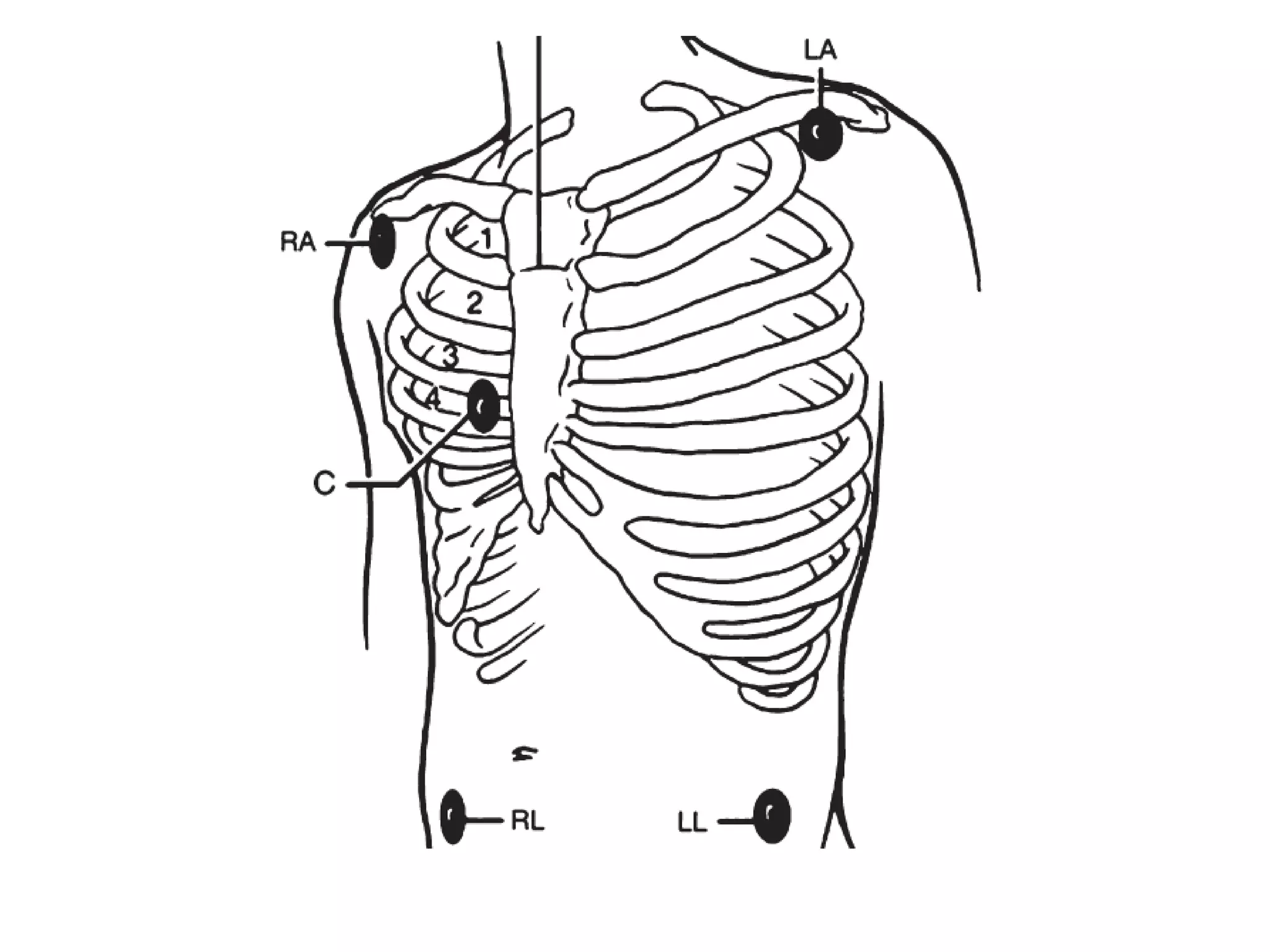
Patient monitoring involves both non-instrumental and instrumental assessment. Non-instrumental monitoring includes visual observation of factors like respiratory pattern, bleeding, and IV lines. Instrumental monitoring provides quantitative data through devices like ECG, blood pressure cuffs, pulse oximetry, capnography, and muscle relaxation monitors. Together, non-instrumental and instrumental monitoring provide clinicians with vital information about patients' physiological status to guide care in settings like operating rooms and intensive care.


![• Auscultation of the Korotkoff sounds
permit estimation of both systolic (SP) and
diastolic (DP)
• blood pressures. MAP can be calculated
using an estimating equation (MAP = DP +
1/3 [SP-DP]).](https://image.slidesharecdn.com/monitoring-120329164509-phpapp02/75/anaesthesia-Monitoring-2-dr-amr-11-2048.jpg)