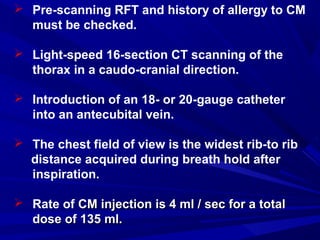
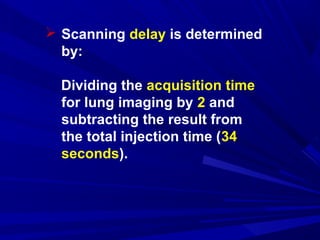
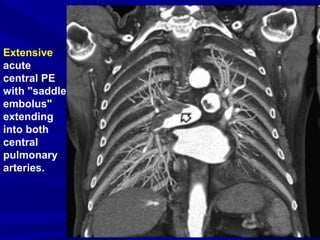
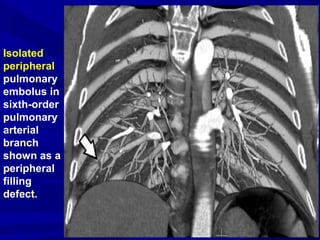
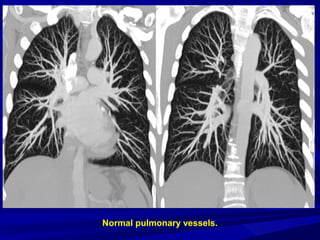
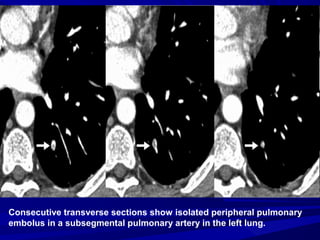
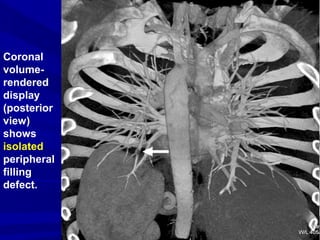
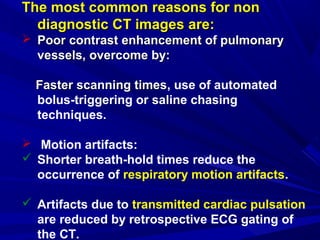
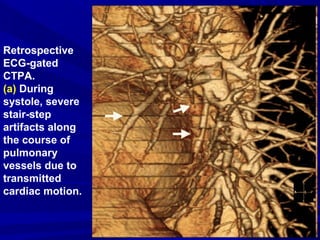
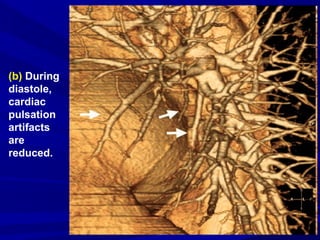
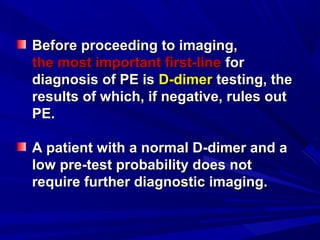
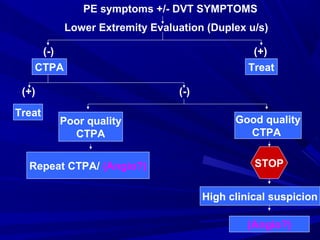
CT Angiography is an important technique for diagnosing pulmonary embolism (PE). It allows direct visualization of blood clots in the lungs. A 16-slice CT scan can cover the entire chest in less than 10 seconds with 1mm resolution, evaluating vessels down to the 6th order branches. While CTPA is fast, non-invasive and highly sensitive and specific, limitations include potential allergic reactions to contrast dye or risks for patients with kidney problems or pregnancy. Proper technique including timing of contrast injection is important to avoid motion artifacts.