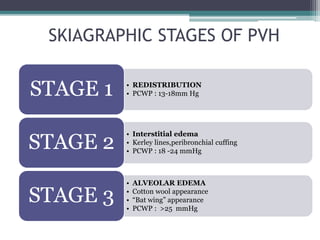
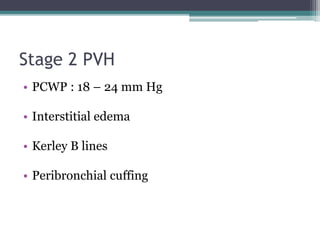
1) Pulmonary venous hypertension (PVH) is classified into 3 stages based on chest x-ray findings and pulmonary capillary wedge pressure (PCWP) levels. Stage 1 is seen at PCWP of 13-18 mmHg and shows redistribution of blood flow. Stage 2 occurs at PCWP of 18-24 mmHg and exhibits interstitial edema and Kerley lines. Stage 3 presents at PCWP over 25 mmHg with alveolar edema and cotton wool appearance.
2) Evaluation of pulmonary hypertension associated with left heart disease (PH-LHD) includes assessing transpulmonary gradient (TPG) and diastolic pressure difference (DPD) via right heart catheterization to determine if the