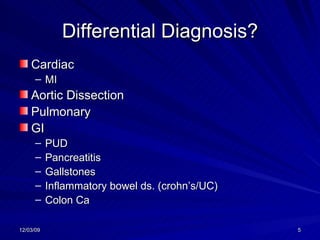
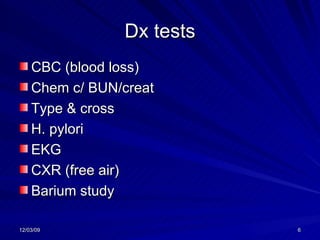
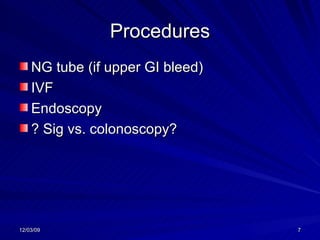
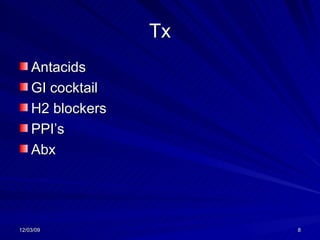
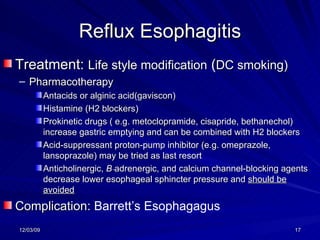
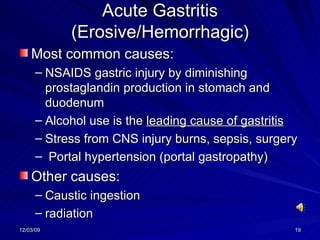
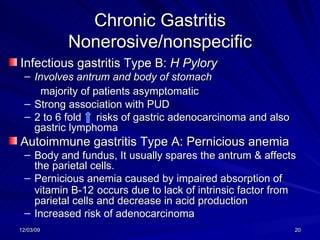
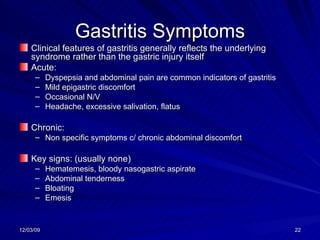
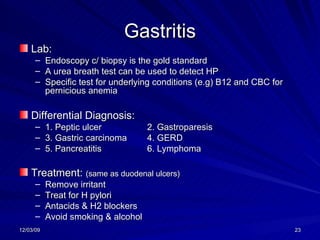
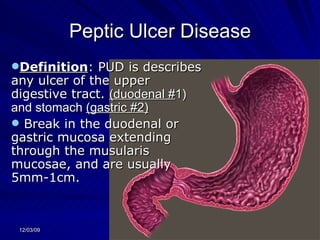
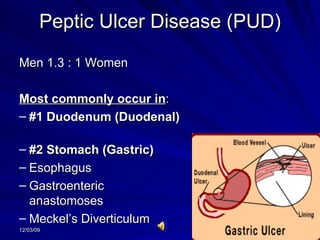
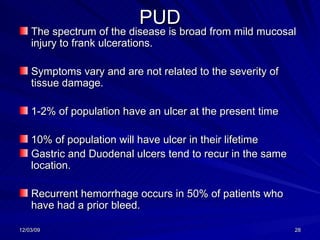
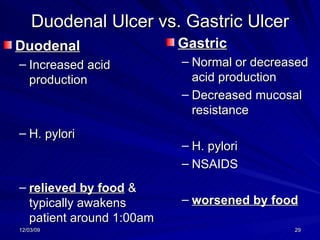
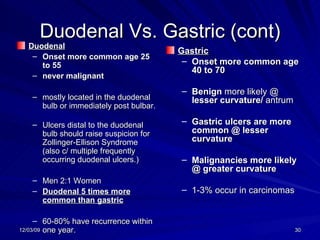
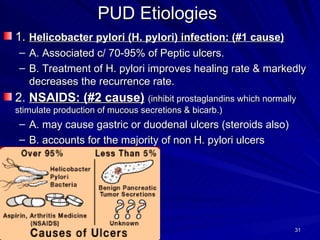
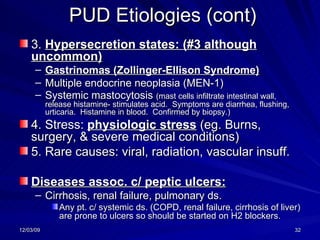
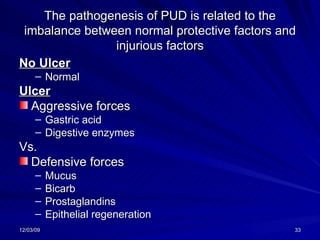
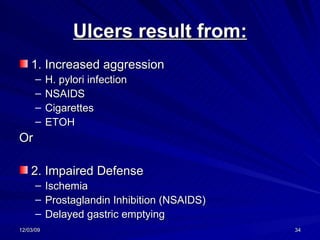
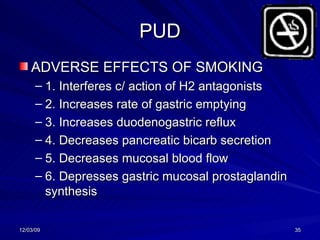
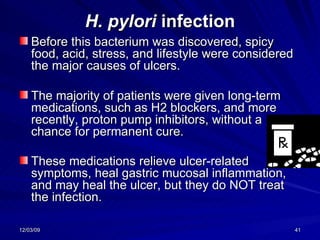
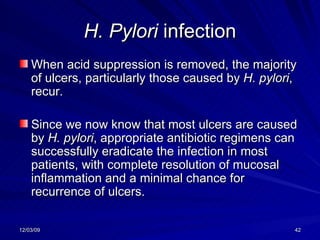
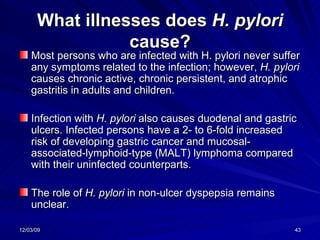
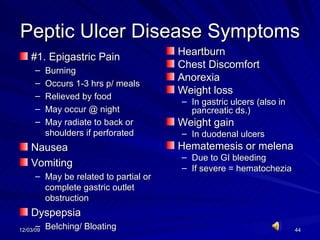
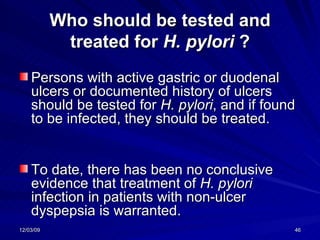
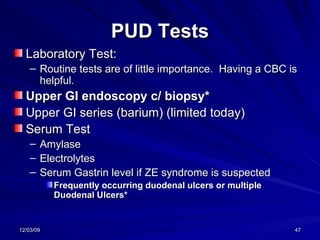
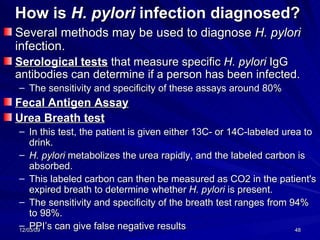
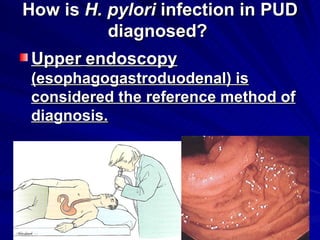
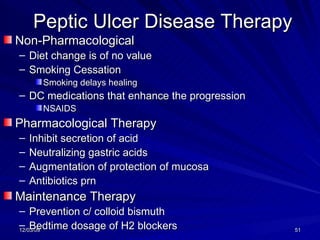
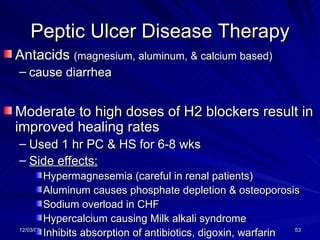
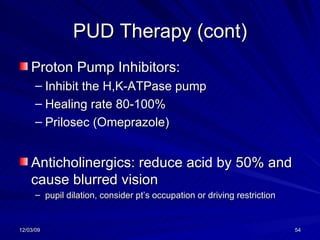
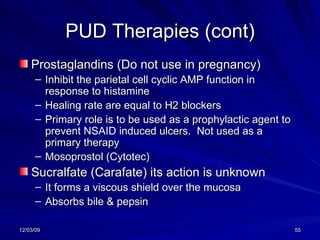
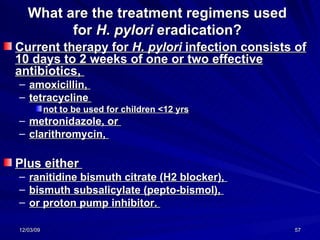
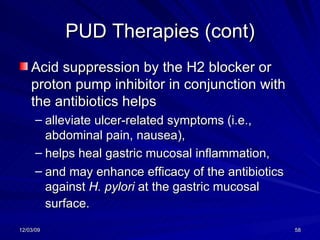
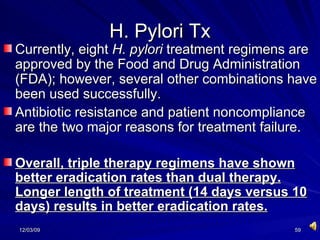
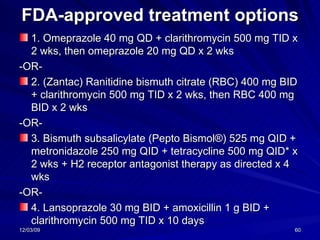
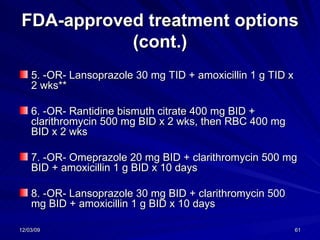
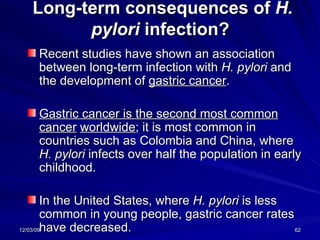
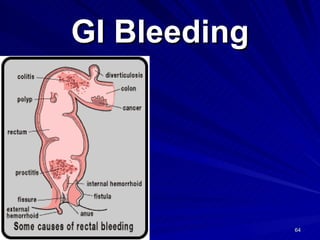
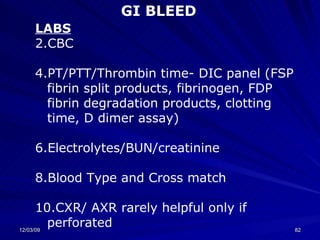
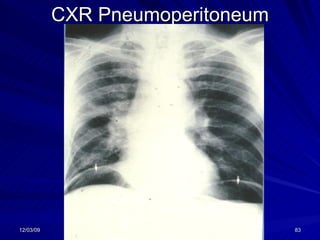
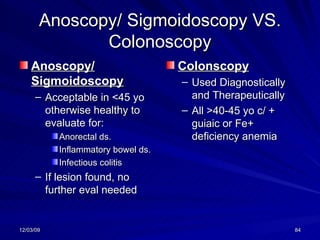
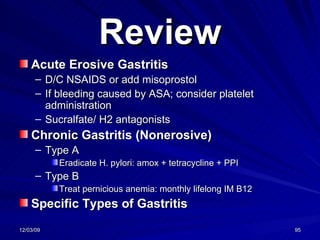
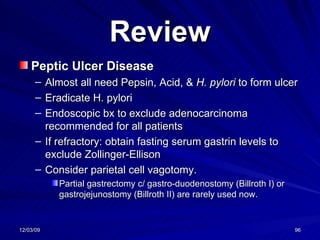
A 55-year-old male presented with epigastric pain for one month that was relieved by food but worsened 1-3 hours later. He also reported fatigue, dyspepsia, bloating, and weight loss. Differential diagnoses included peptic ulcer disease, pancreatitis, and gallstones. Recommended tests included a CBC, chemistries, H. pylori testing, EKG, CXR, and possible endoscopy or barium study. Treatment options included antacids, H2 blockers, PPIs, and antibiotics.