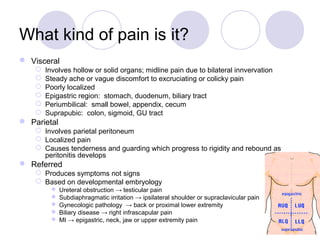
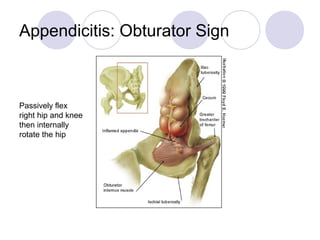
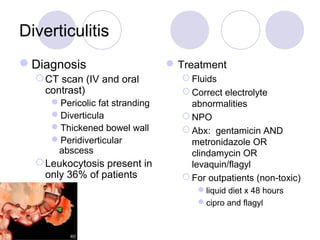
This document is a lecture covering the evaluation and management of acute abdominal pain in emergency medicine, focusing on a 24-year-old male patient with right lower quadrant pain. It discusses the differential diagnoses, examination techniques, and key conditions such as appendicitis, pancreatitis, and cholecystitis, including their presentations and management strategies. Emphasis is placed on the importance of thorough history-taking, physical examination, and appropriate use of imaging and lab tests to guide diagnosis and treatment.