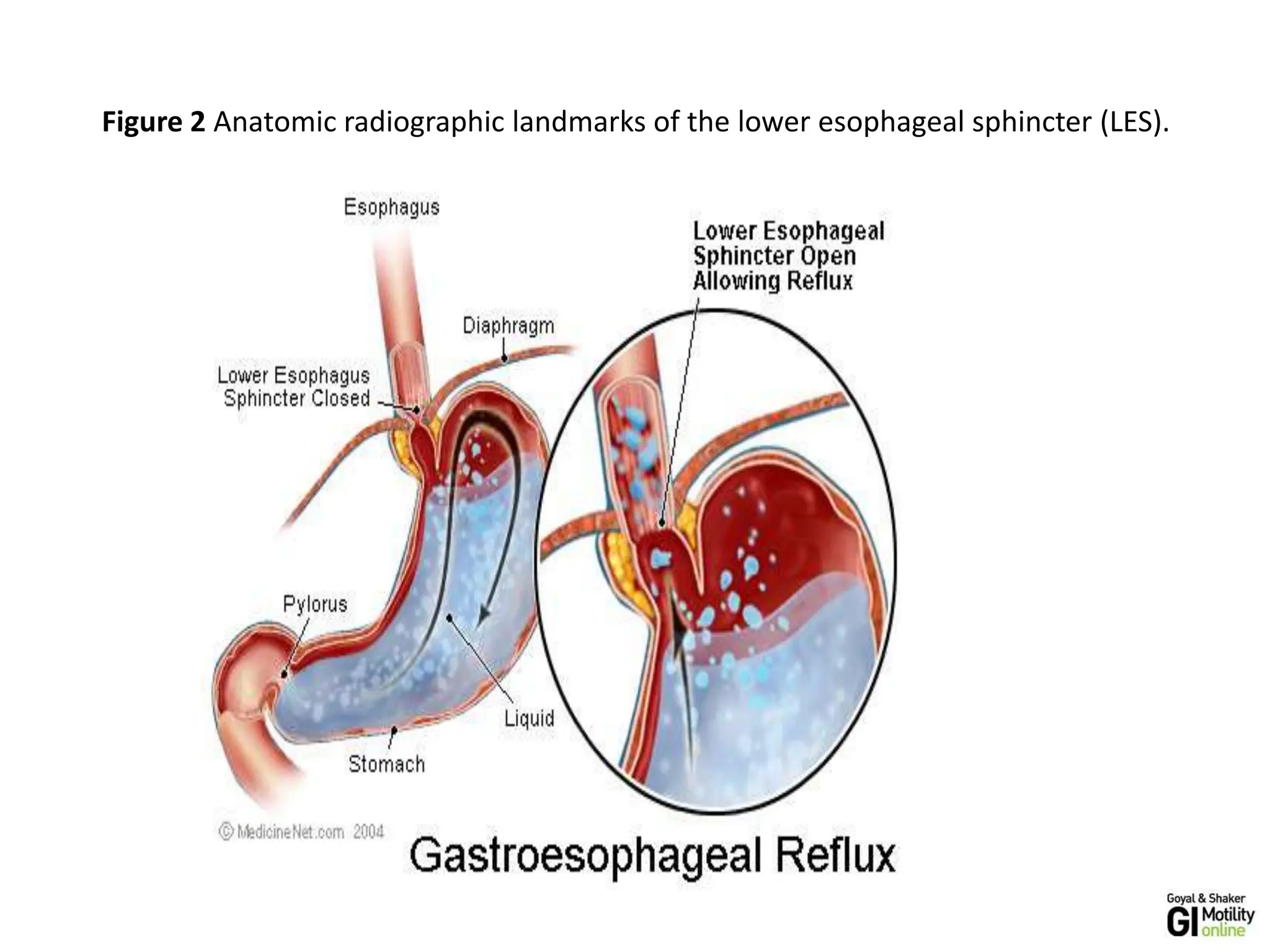
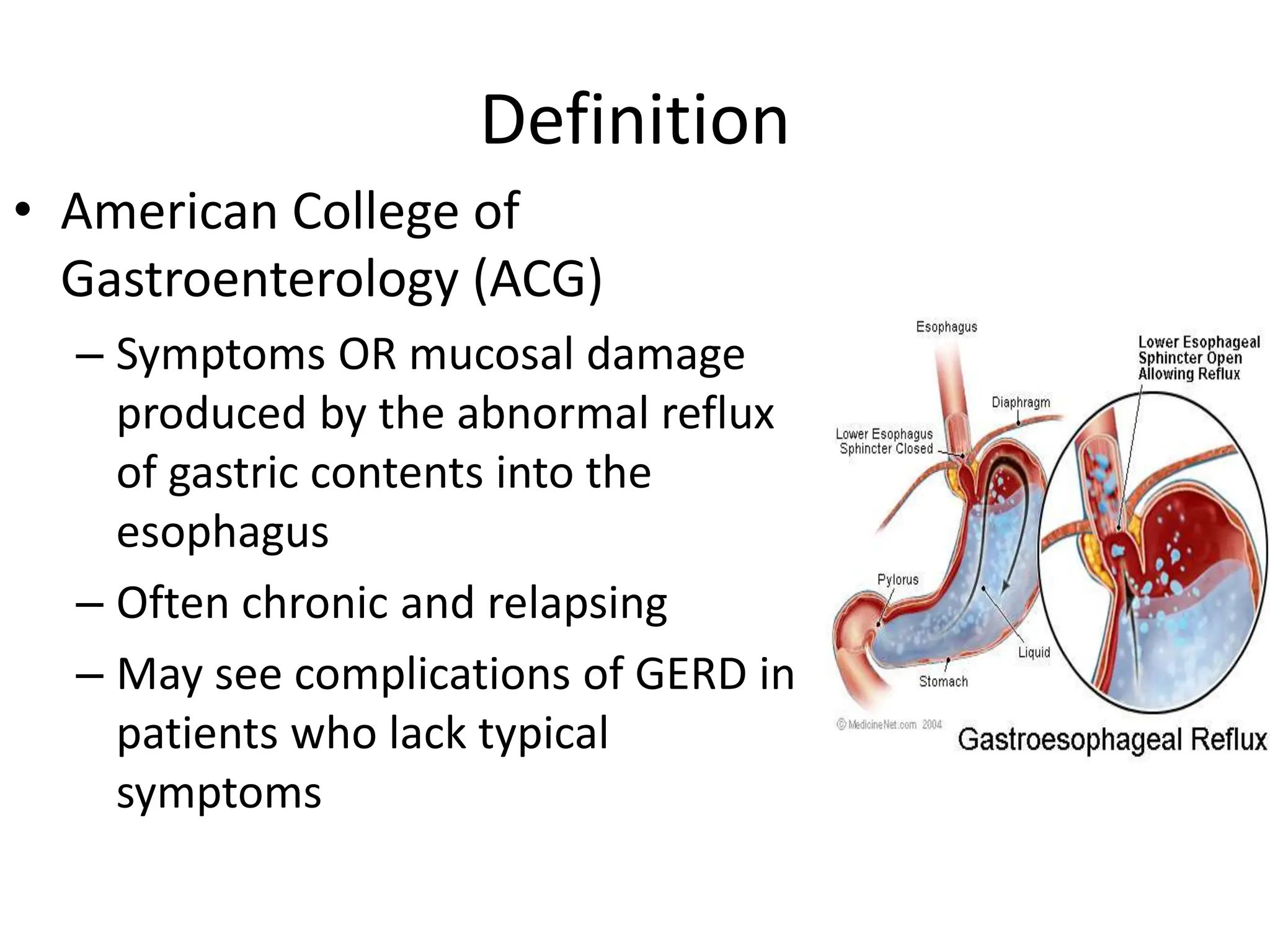
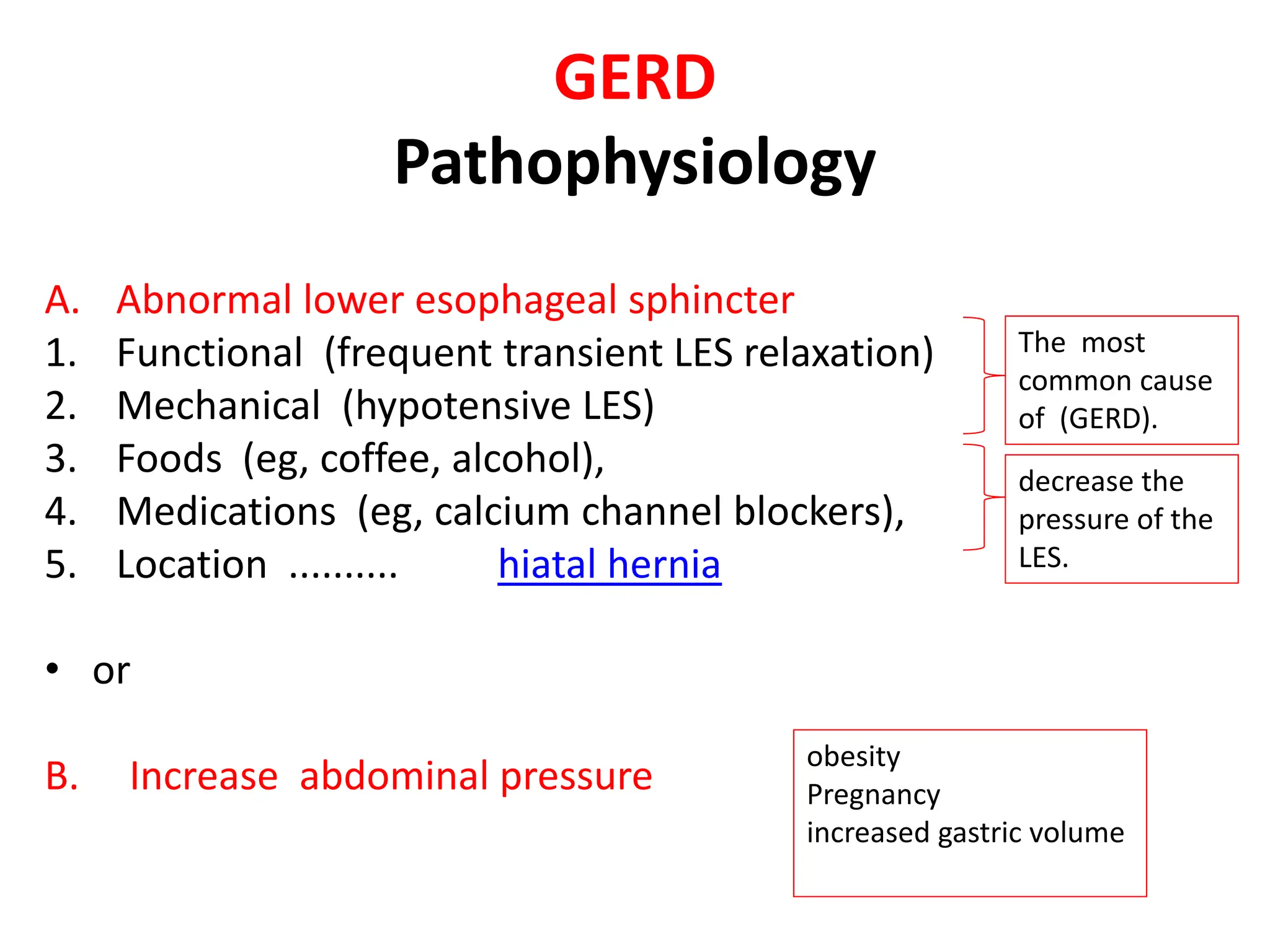
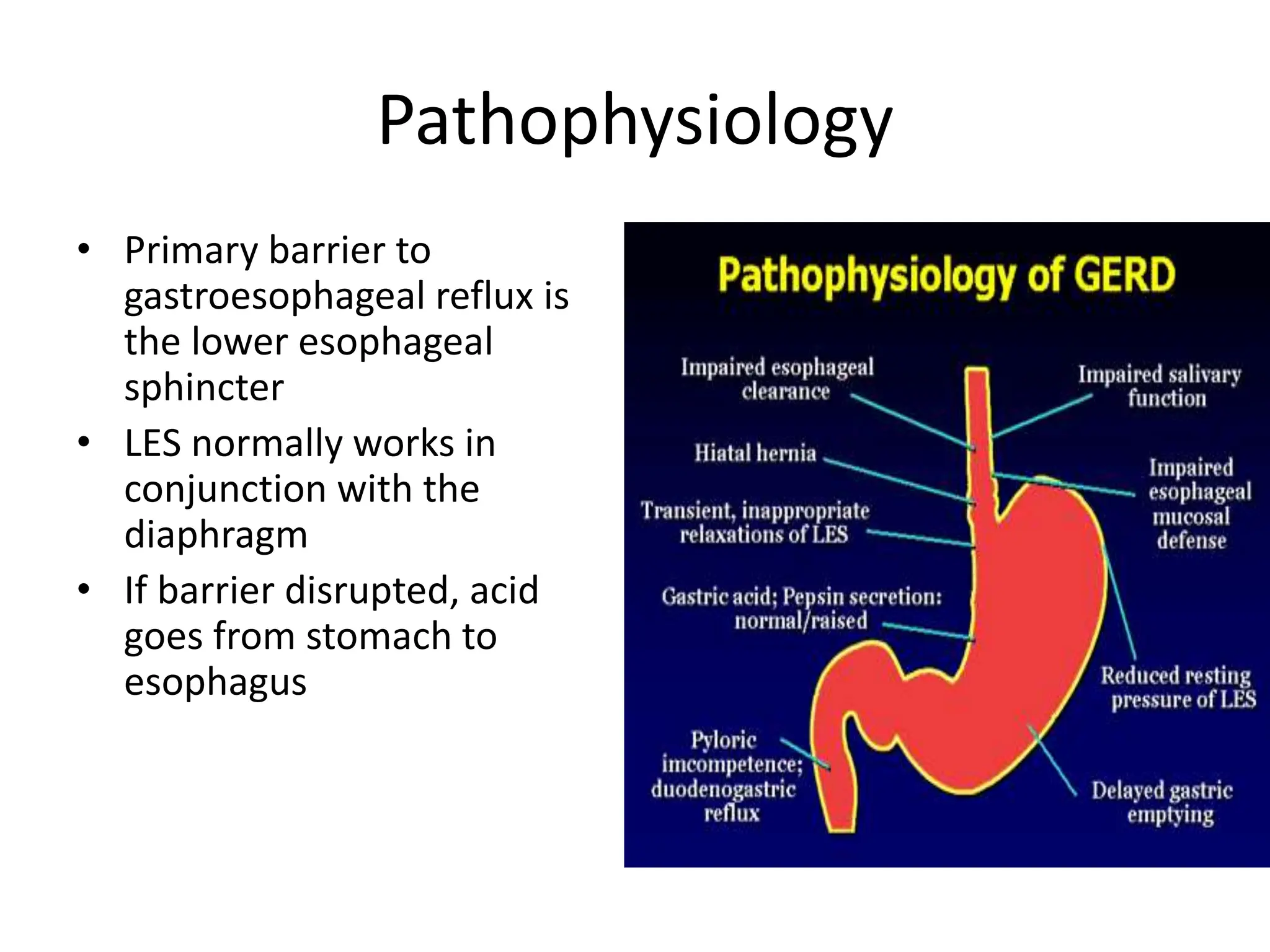
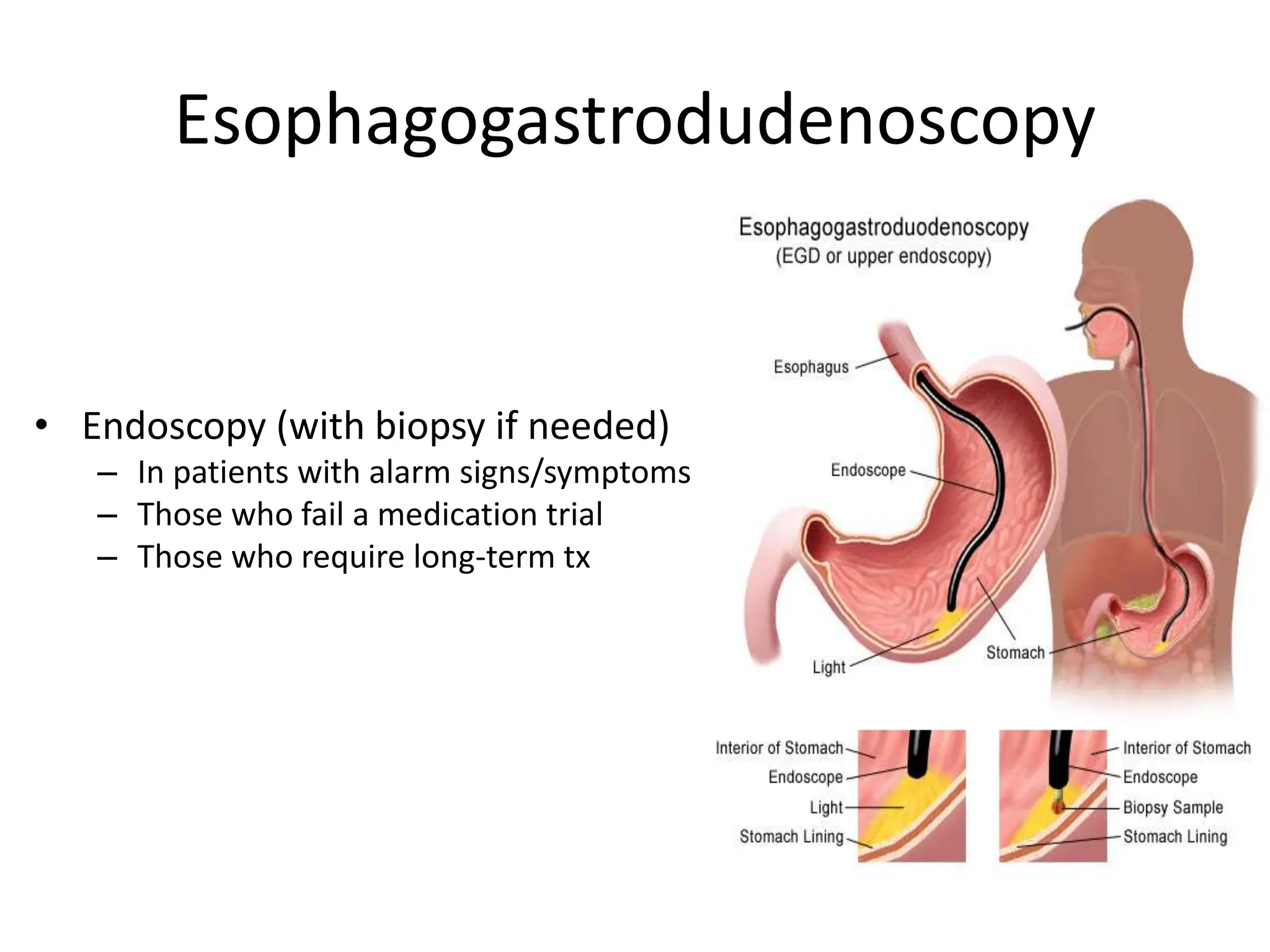
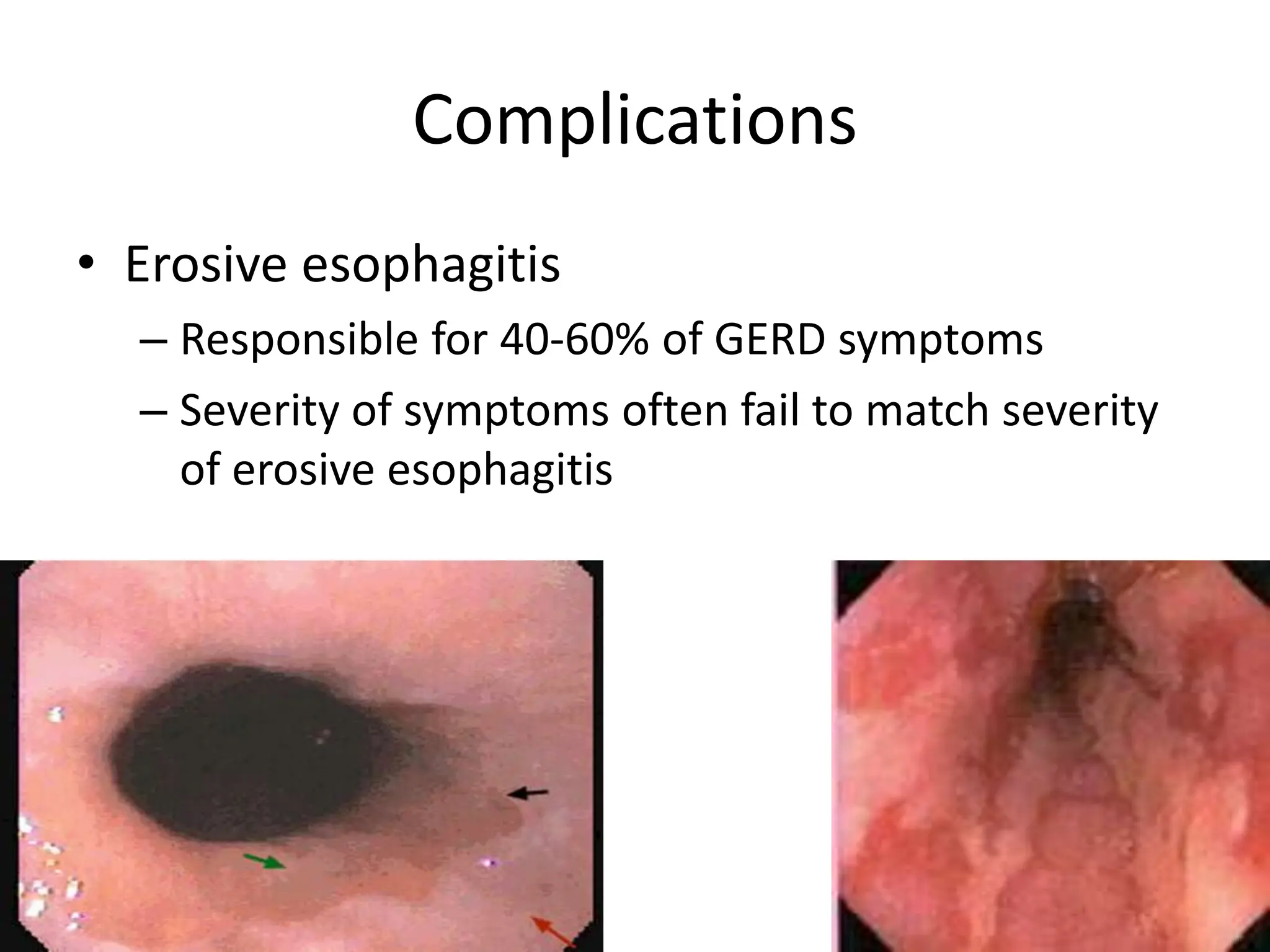
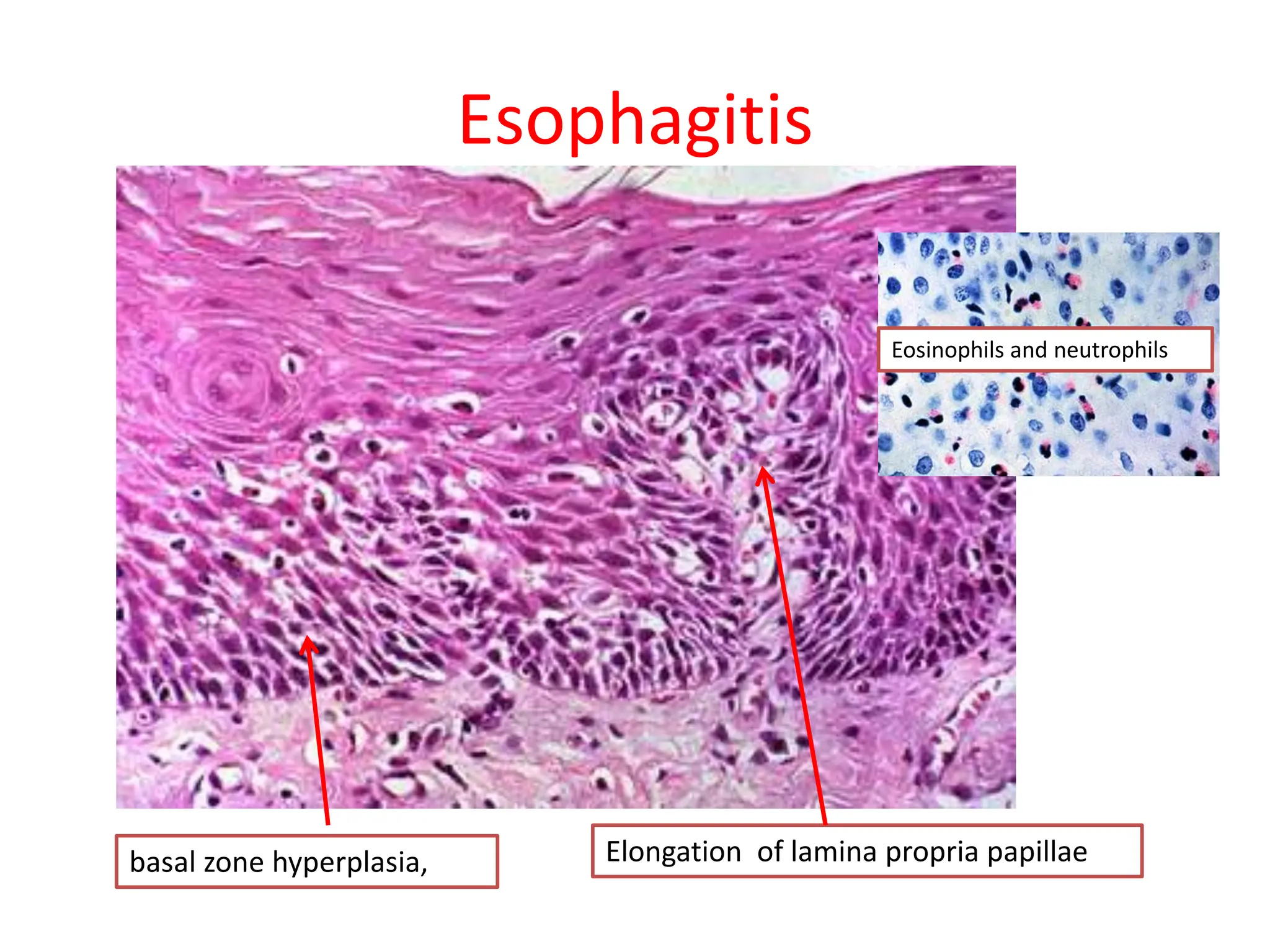
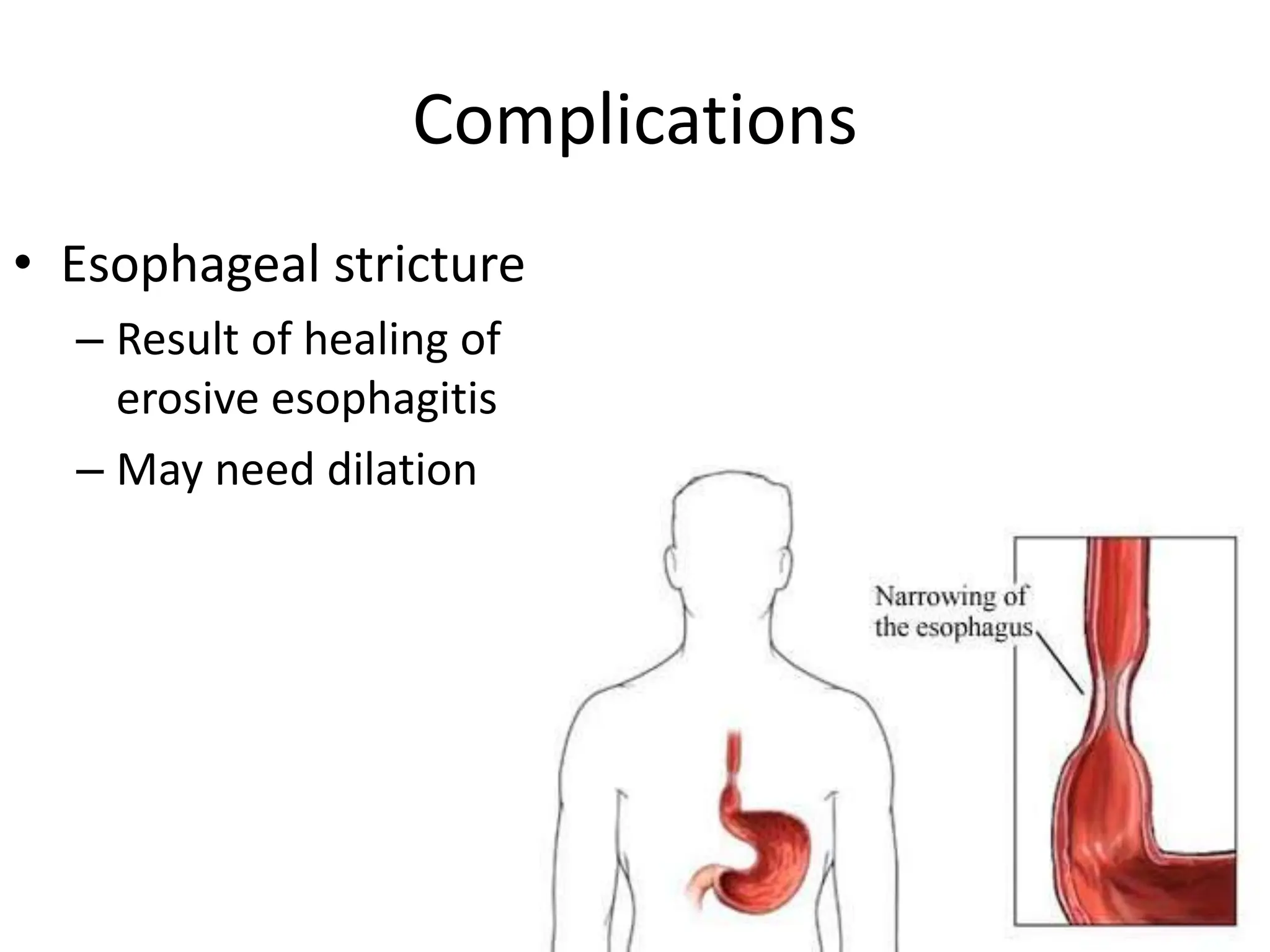
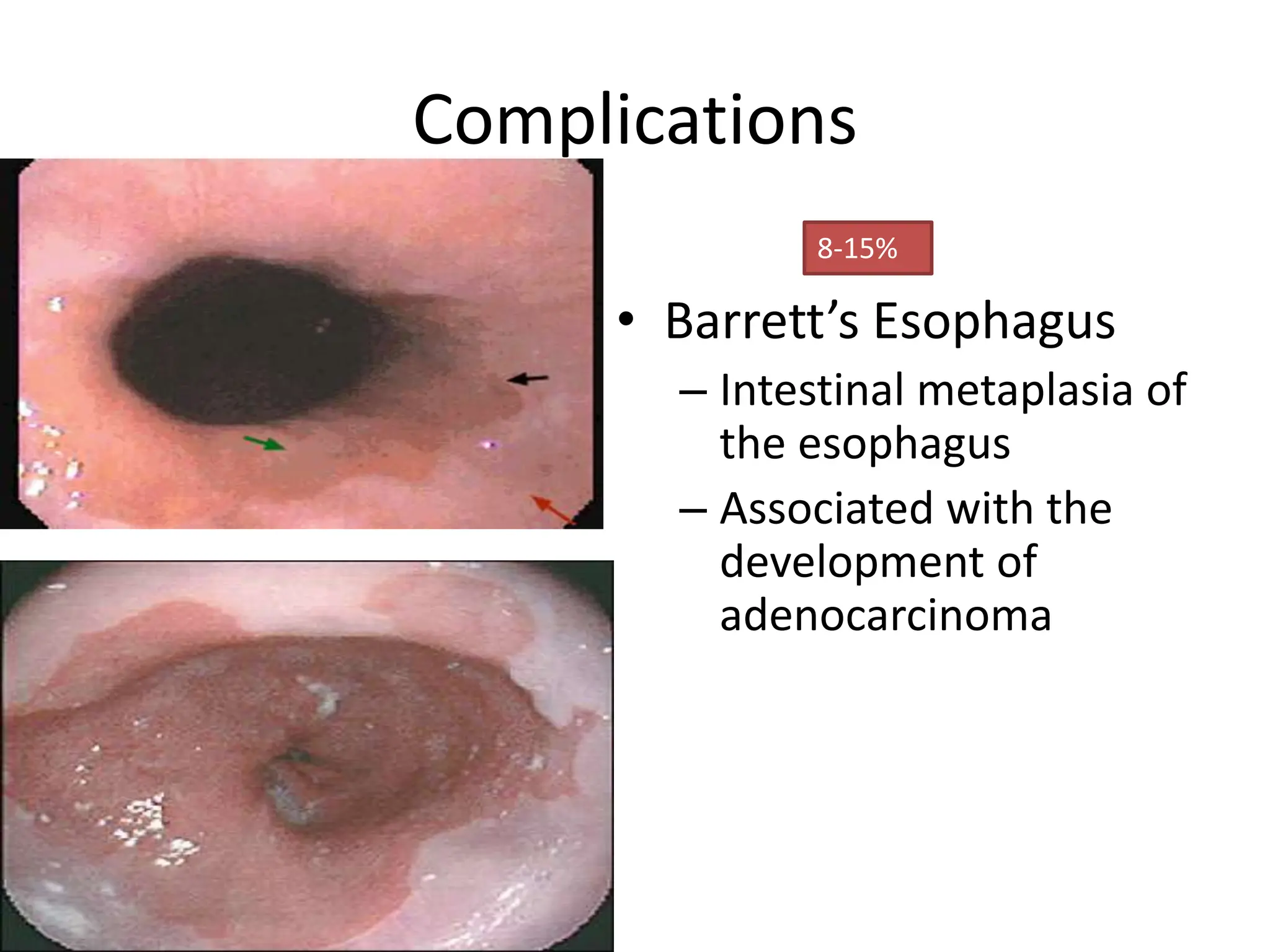
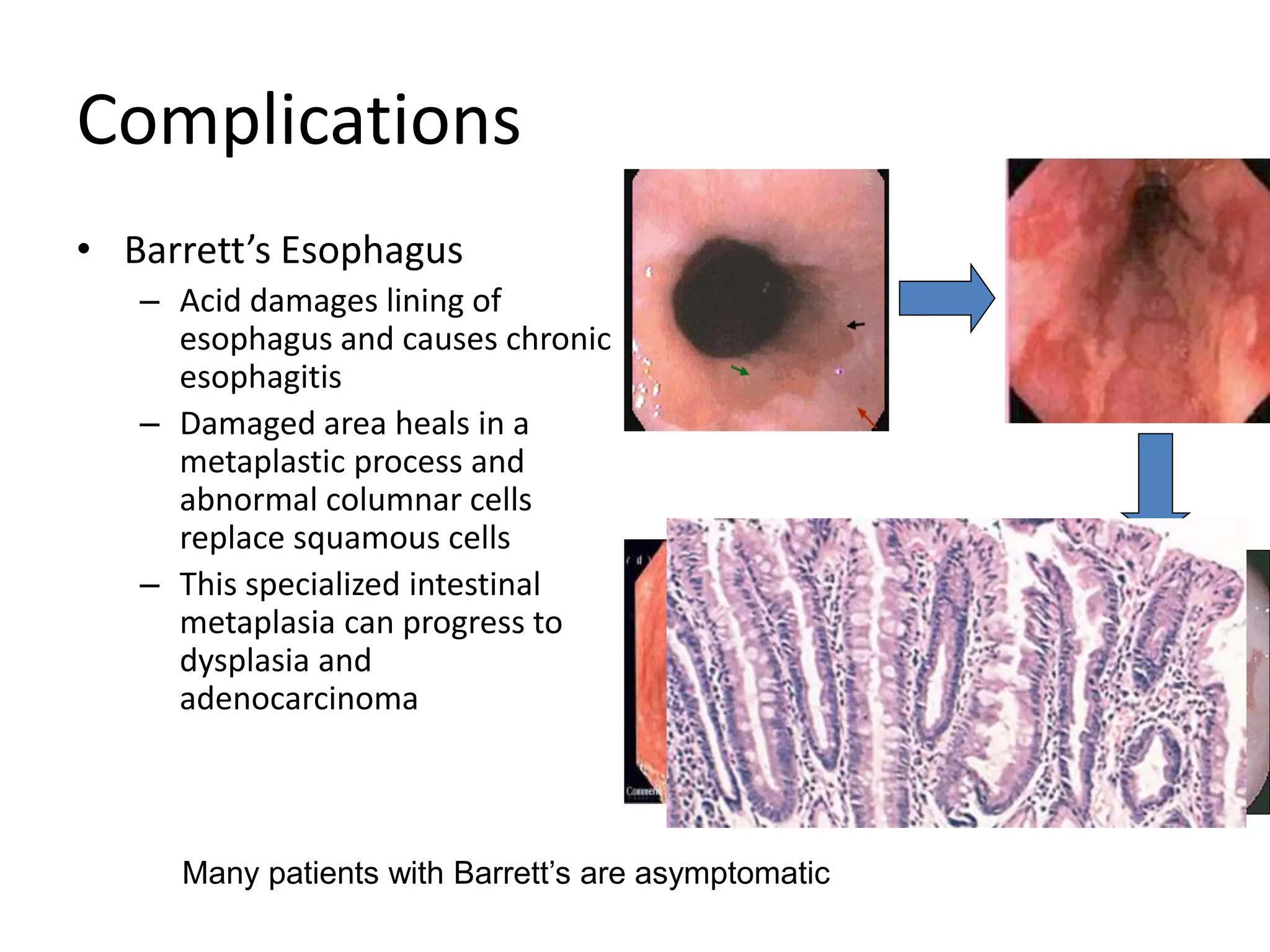
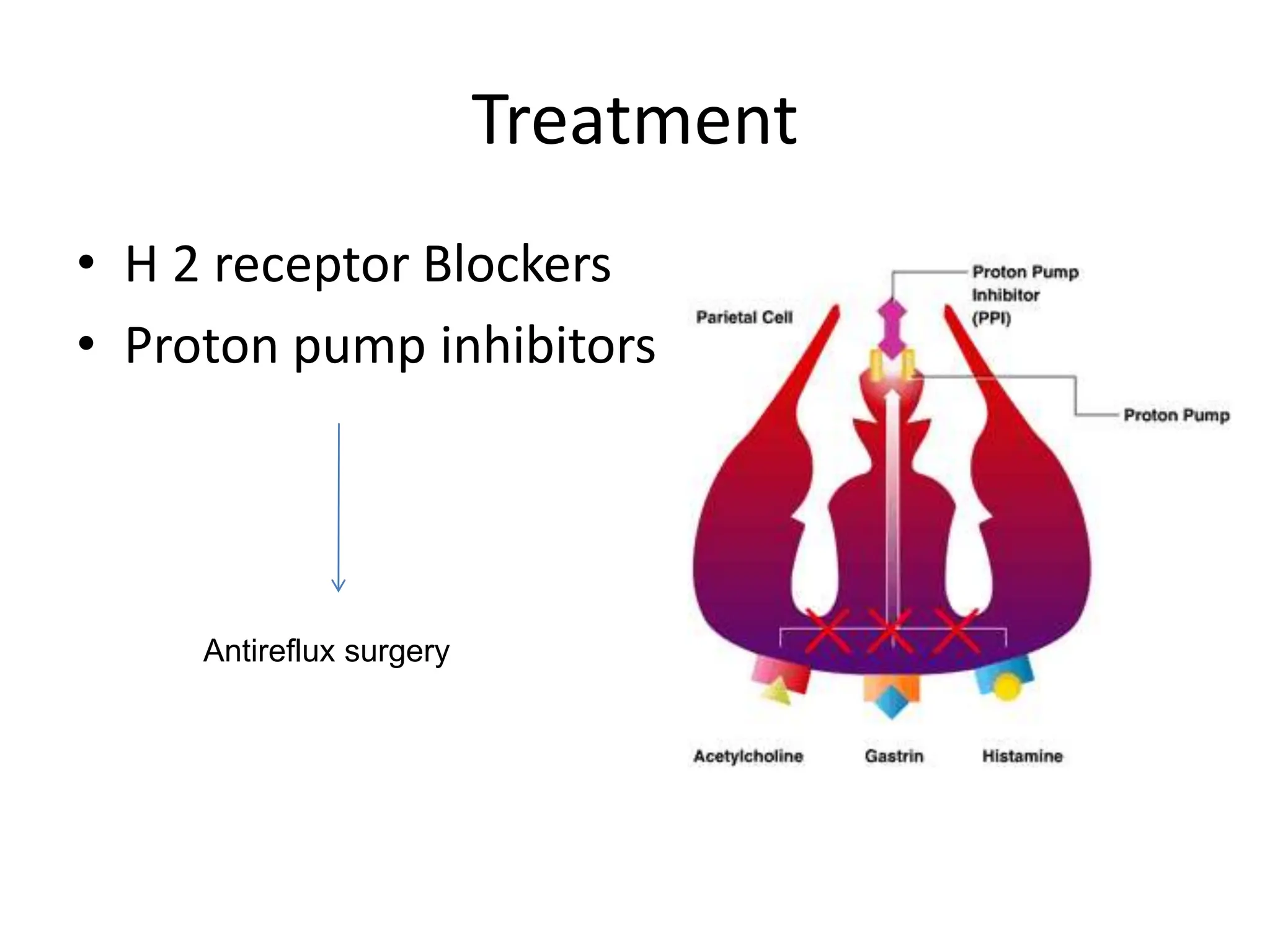
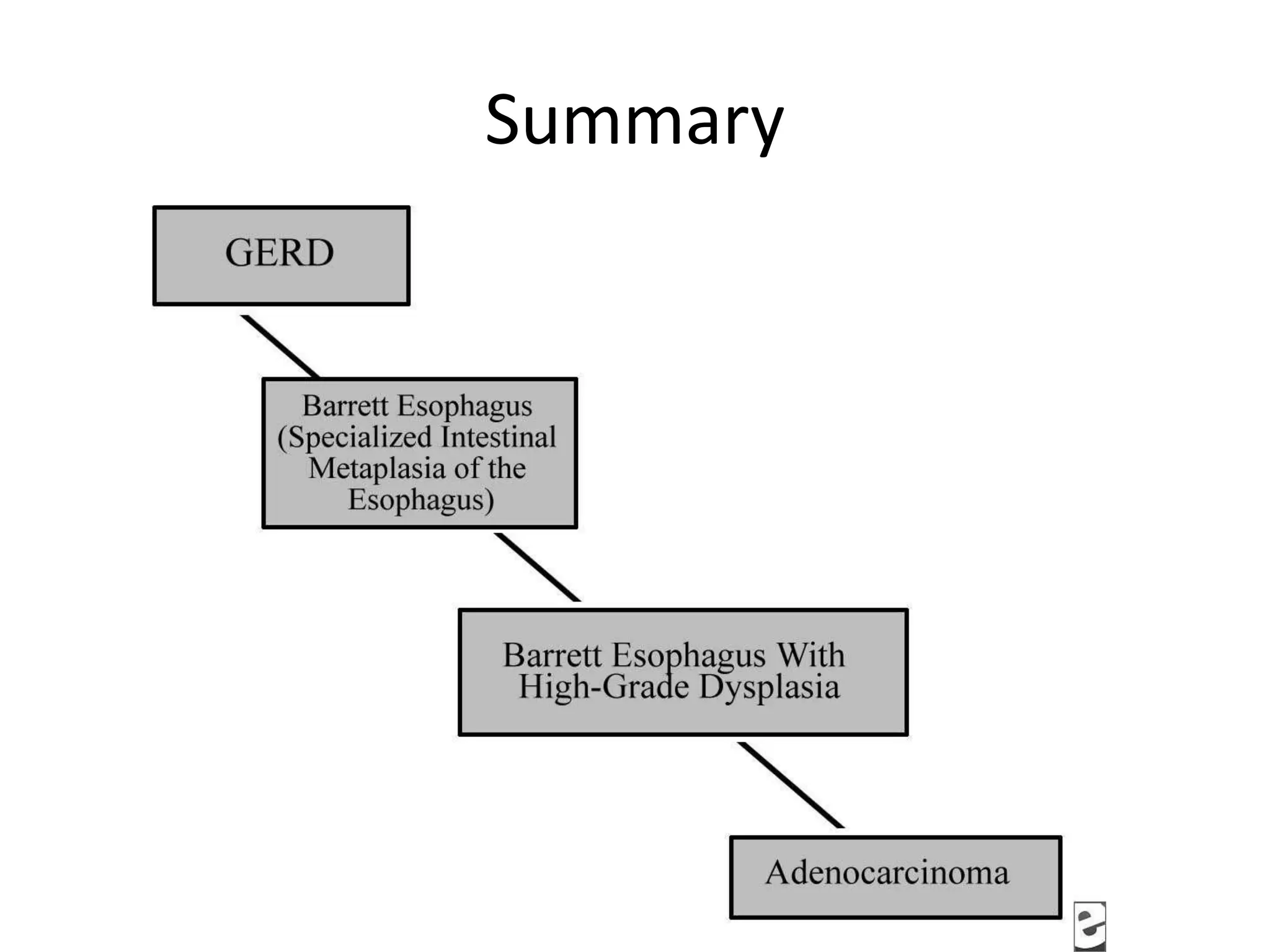
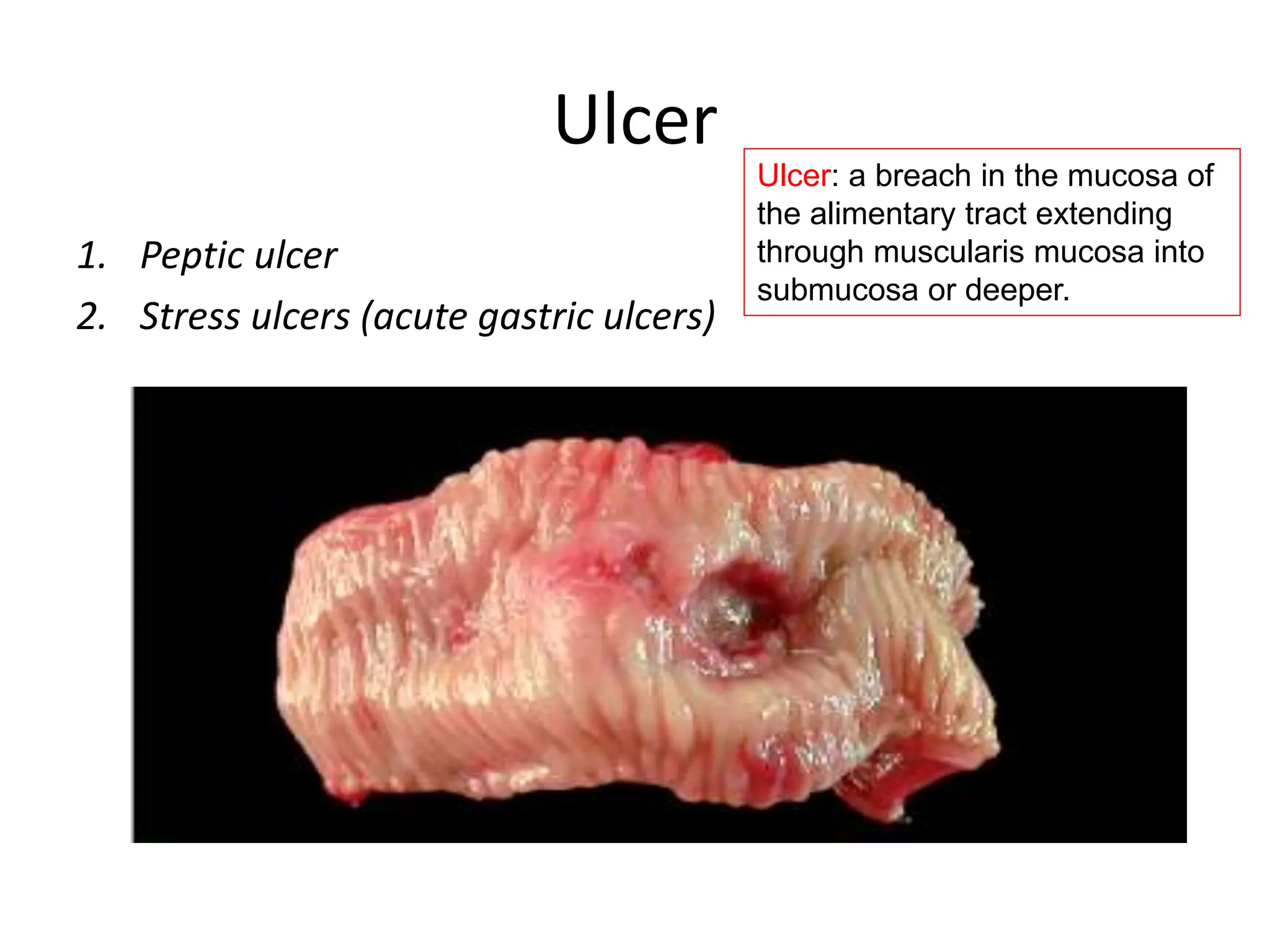
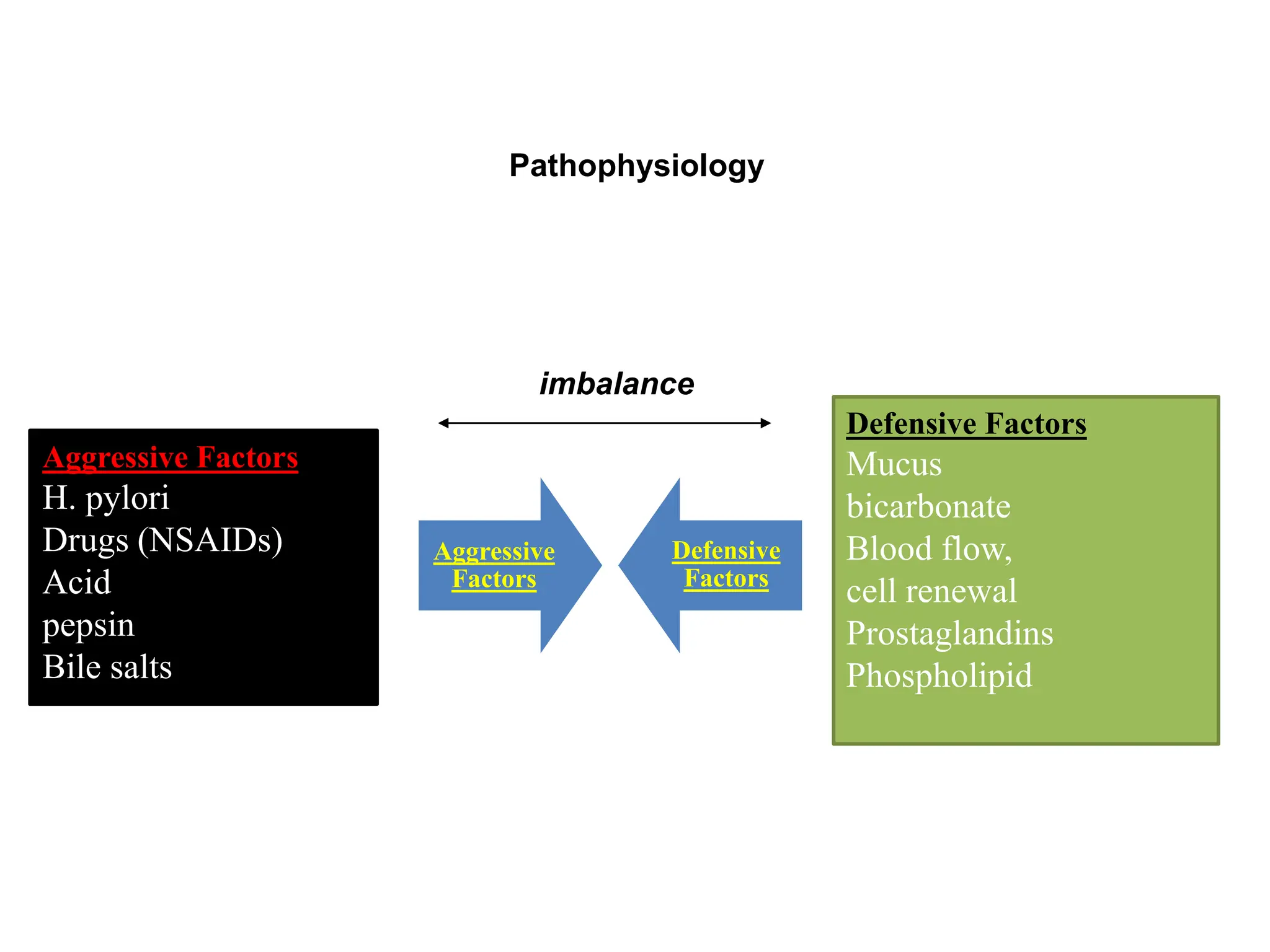
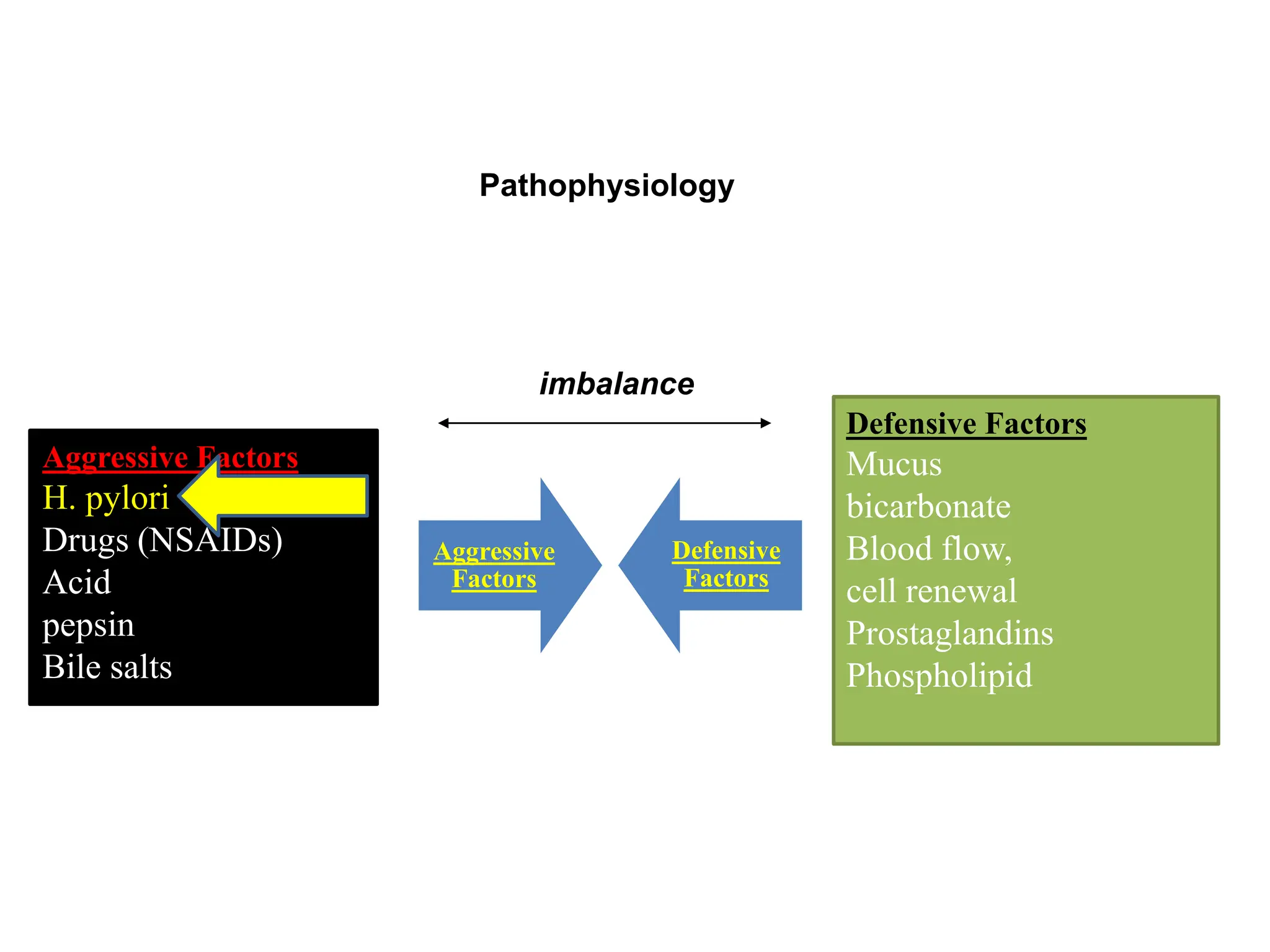
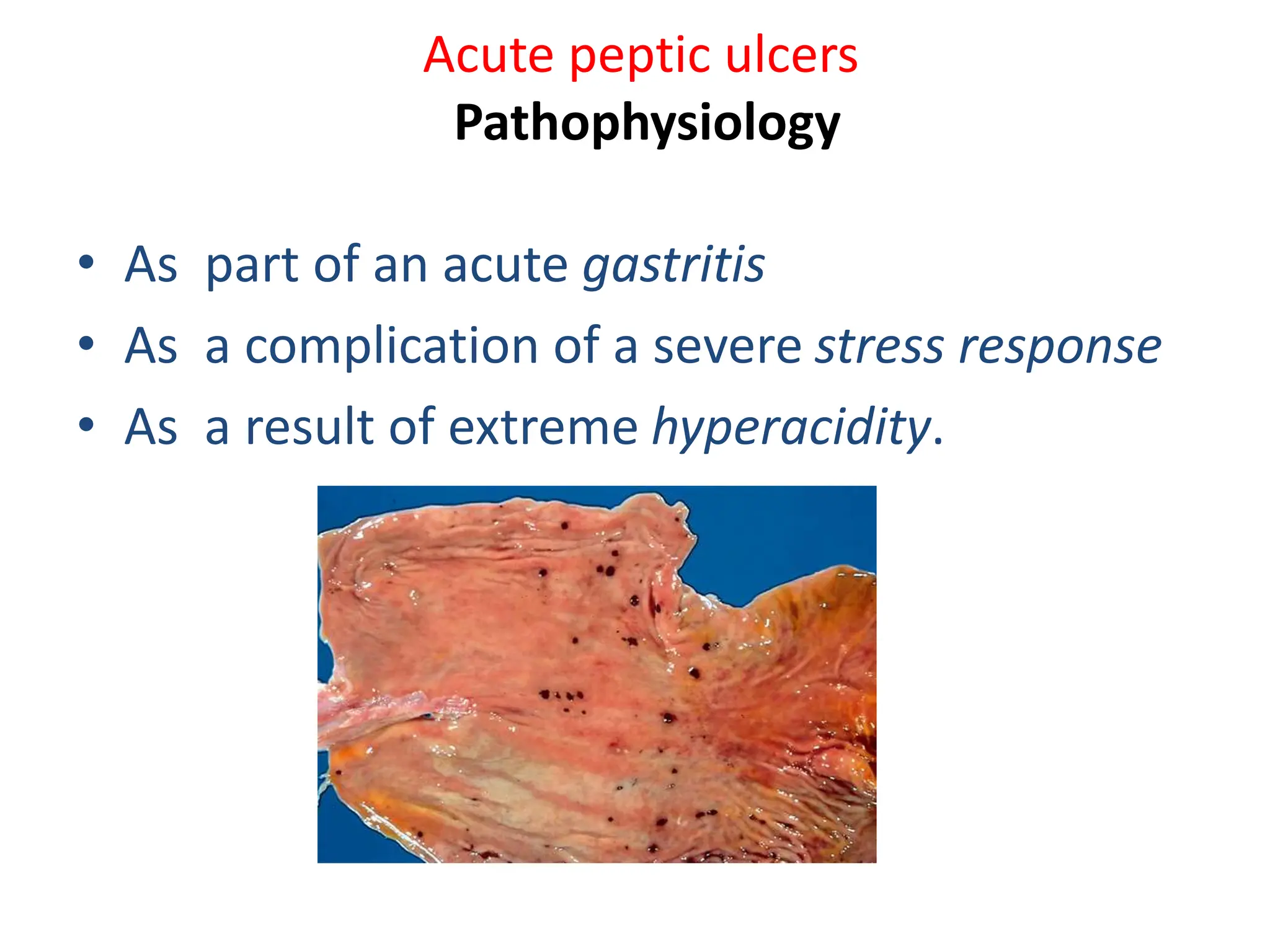
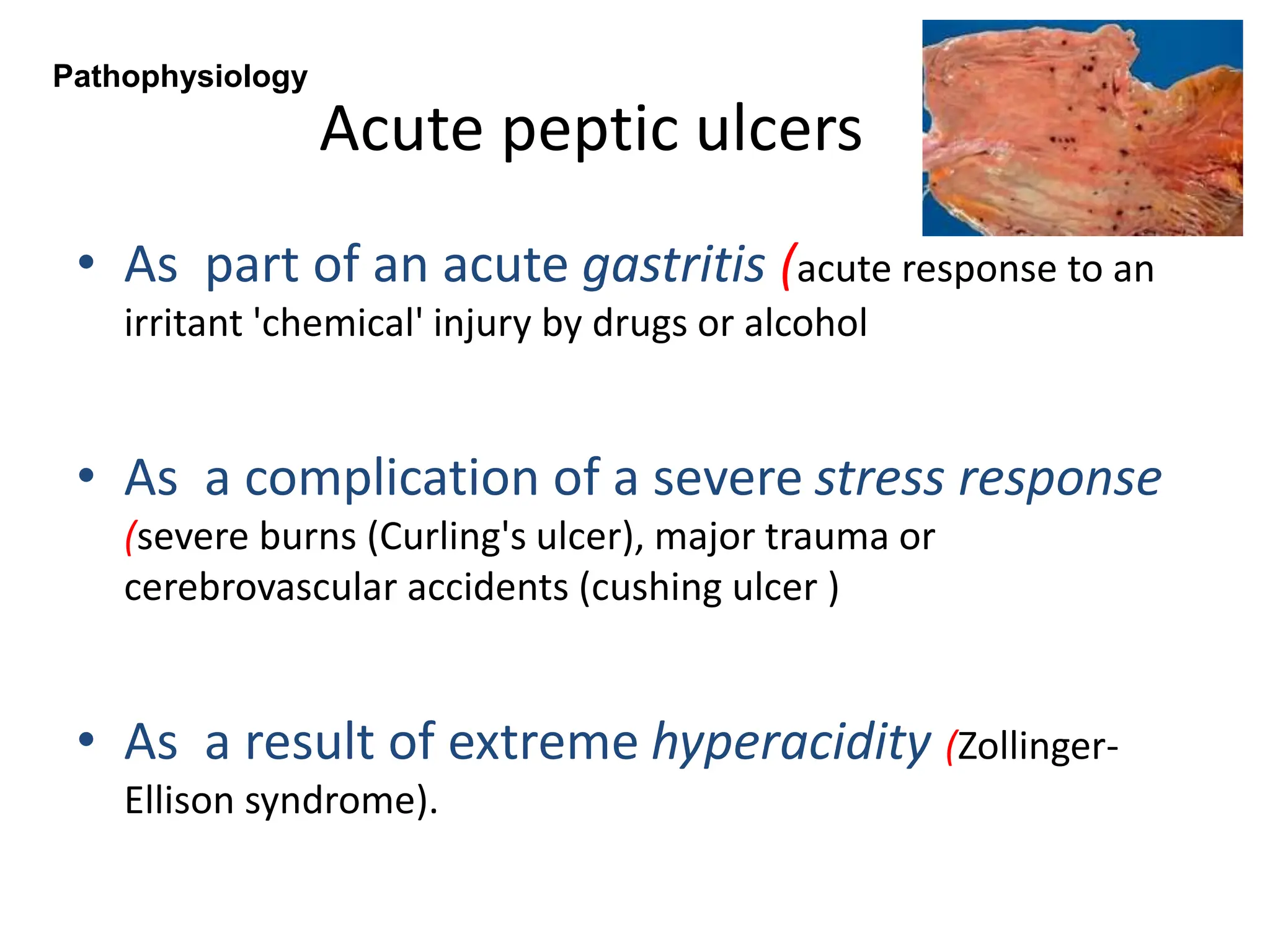
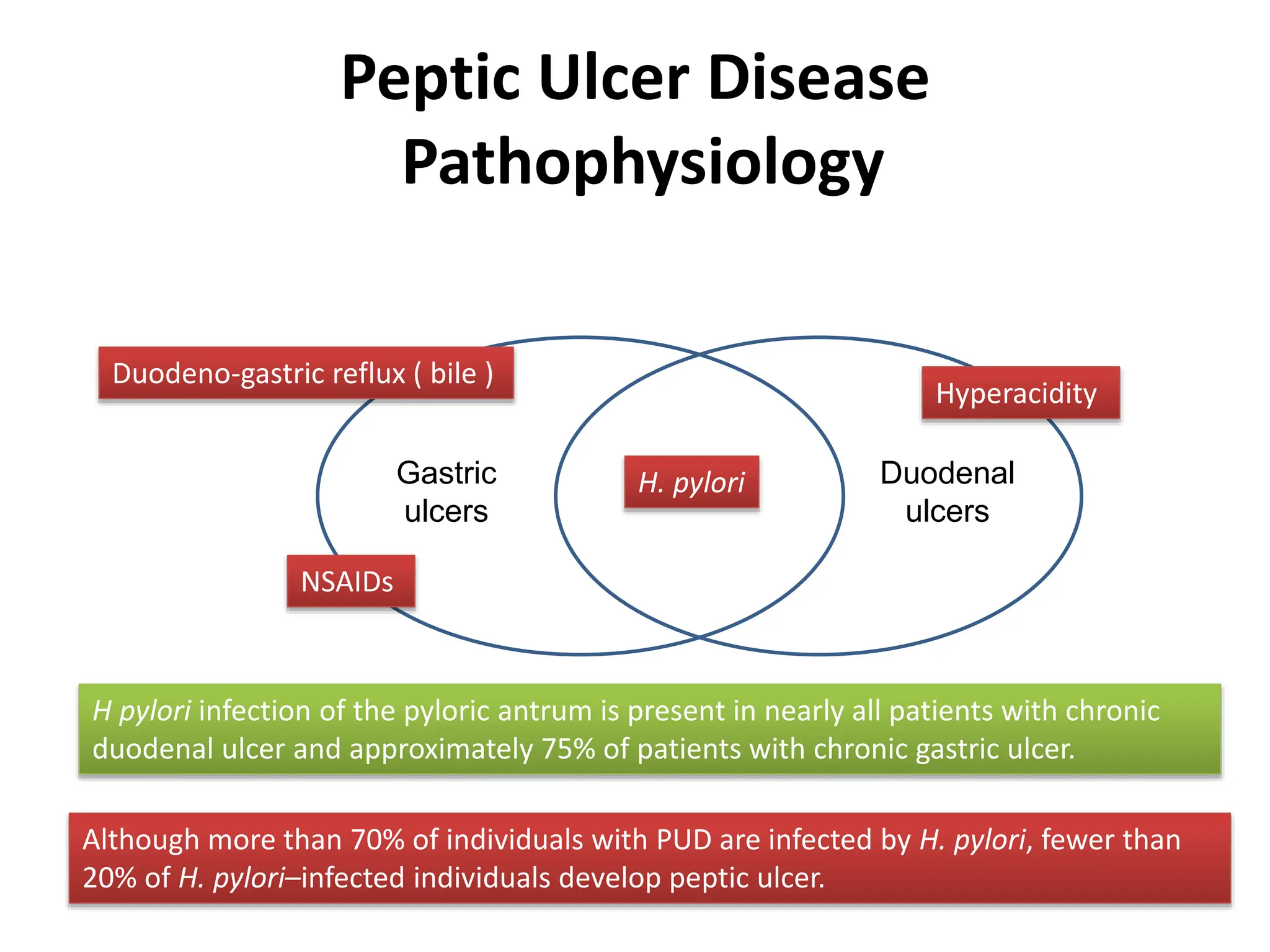
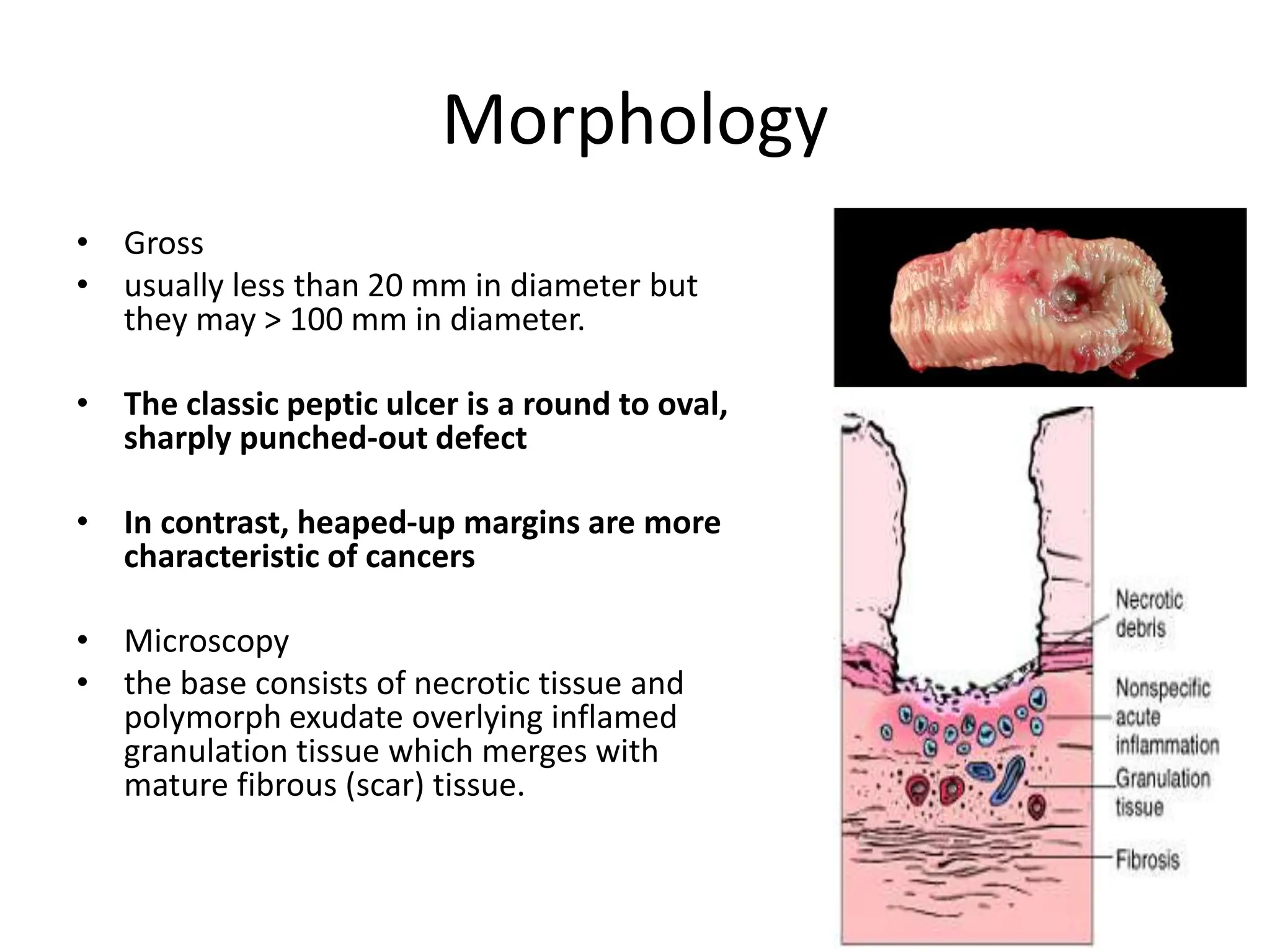
The document comprises lectures on gastro-esophageal reflux disease (GERD) and peptic ulcer disease, covering definitions, pathophysiology, clinical features, diagnostic evaluations, and treatment methods. It highlights the distinction between physiological and pathological GERD, along with the common symptoms, causes, and complications related to both conditions. Treatment approaches for peptic ulcers focus on H. pylori eradication and acid suppression therapies.