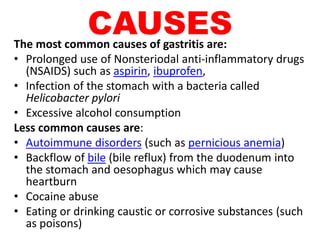
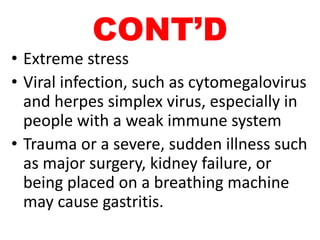
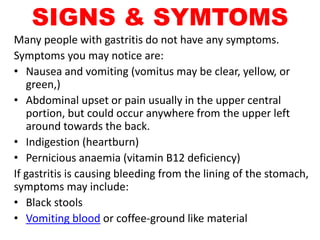
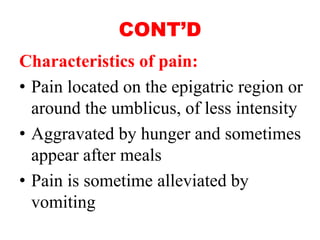
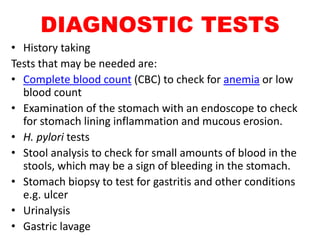
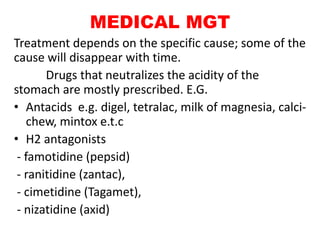
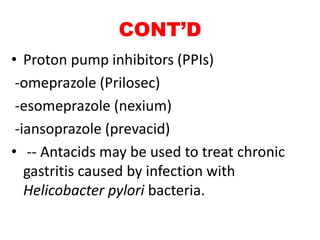
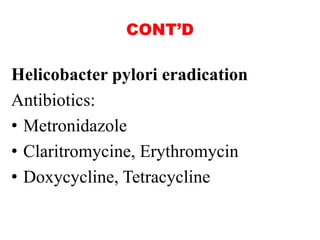
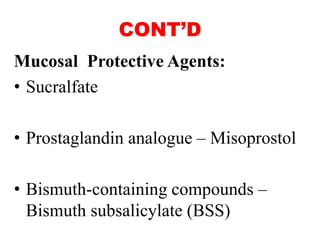
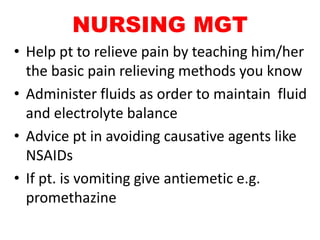
This document provides an outline on gastritis, including its definition, causes, signs and symptoms, diagnostic tests, medical and nursing management, prevention, and complications. Gastritis is defined as inflammation of the stomach lining and can be acute or chronic. Common causes include NSAID use, H. pylori infection, alcohol, and stress. Symptoms may include nausea, abdominal pain, and bleeding. Tests used for diagnosis include endoscopy, blood tests, stool tests, and biopsy. Treatment focuses on reducing acid and treating underlying causes, such as antibiotics for H. pylori. Nursing care includes relieving pain, maintaining nutrition and hydration, administering medications correctly, and educating on lifestyle changes and symptom monitoring