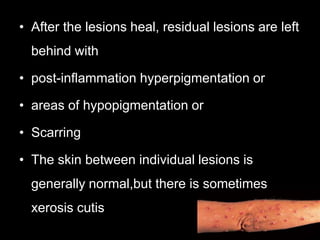
Prurigo is a group of skin diseases characterized by intensely itchy papules or nodules without an identifiable local cause. It is caused by severe chronic itching leading to repetitive scratching and skin irritation. This results in a lymphocyte-rich inflammatory infiltrate, activated keratinocytes and sensory nerves, and increased collagen tissue.
Prurigo nodularis specifically presents as intensely itchy nodules on the extremities. Histology shows hyperkeratosis, acanthosis, and proliferation of cutaneous nerves and fibroblasts. Treatment focuses on eliminating pruritus through antipruritic medications and phototherapy to break the itch-scratch cycle and reduce inflammation.