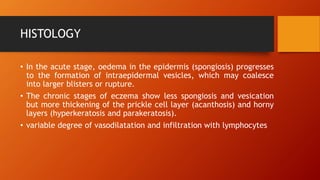
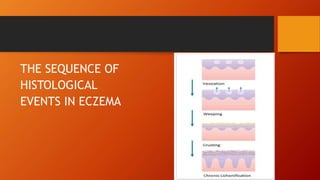
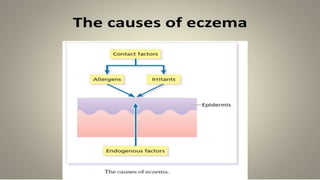
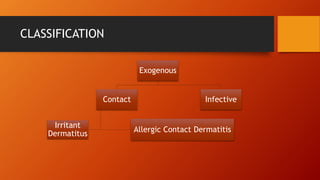
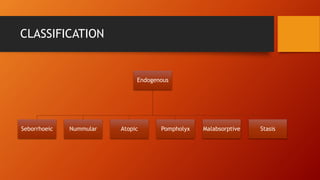
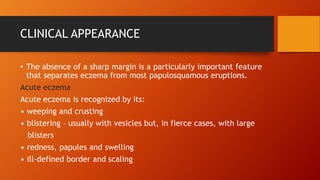
The document provides a comprehensive overview of eczema, including its definition, histology, classification, clinical manifestations, differential diagnosis, complications, investigations, and treatment options. Eczema is characterized by itchy, erythematous eruptions and can be classified into different forms such as allergic contact dermatitis and atopic eczema. Treatment varies by type and severity, with options including corticosteroids, calcineurin inhibitors, and systemic therapies.