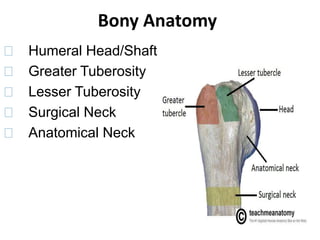
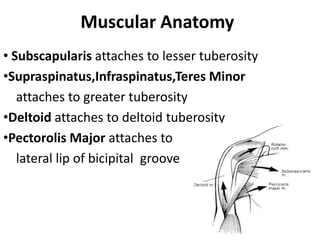
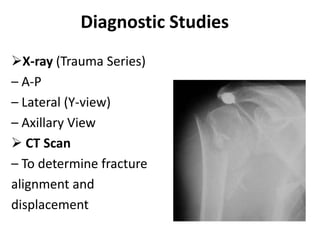
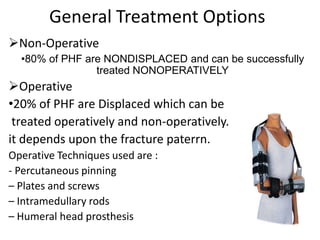
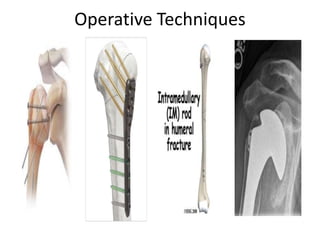
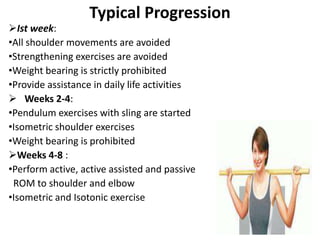
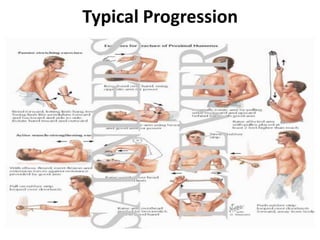
Proximal humerus fractures are fractures near the top of the upper arm bone. They commonly occur in older patients from falls and make up 4-5% of all fractures. Diagnosis is made using x-rays and sometimes CT scans. Treatment depends on the level of displacement but may involve non-operative methods like slings or operative techniques like plating or nailing. Early rehabilitation focusing on range of motion and strength is important to prevent stiffness and regain function. Complications can include stiffness, malunion, avascular necrosis, and heterotopic ossification.