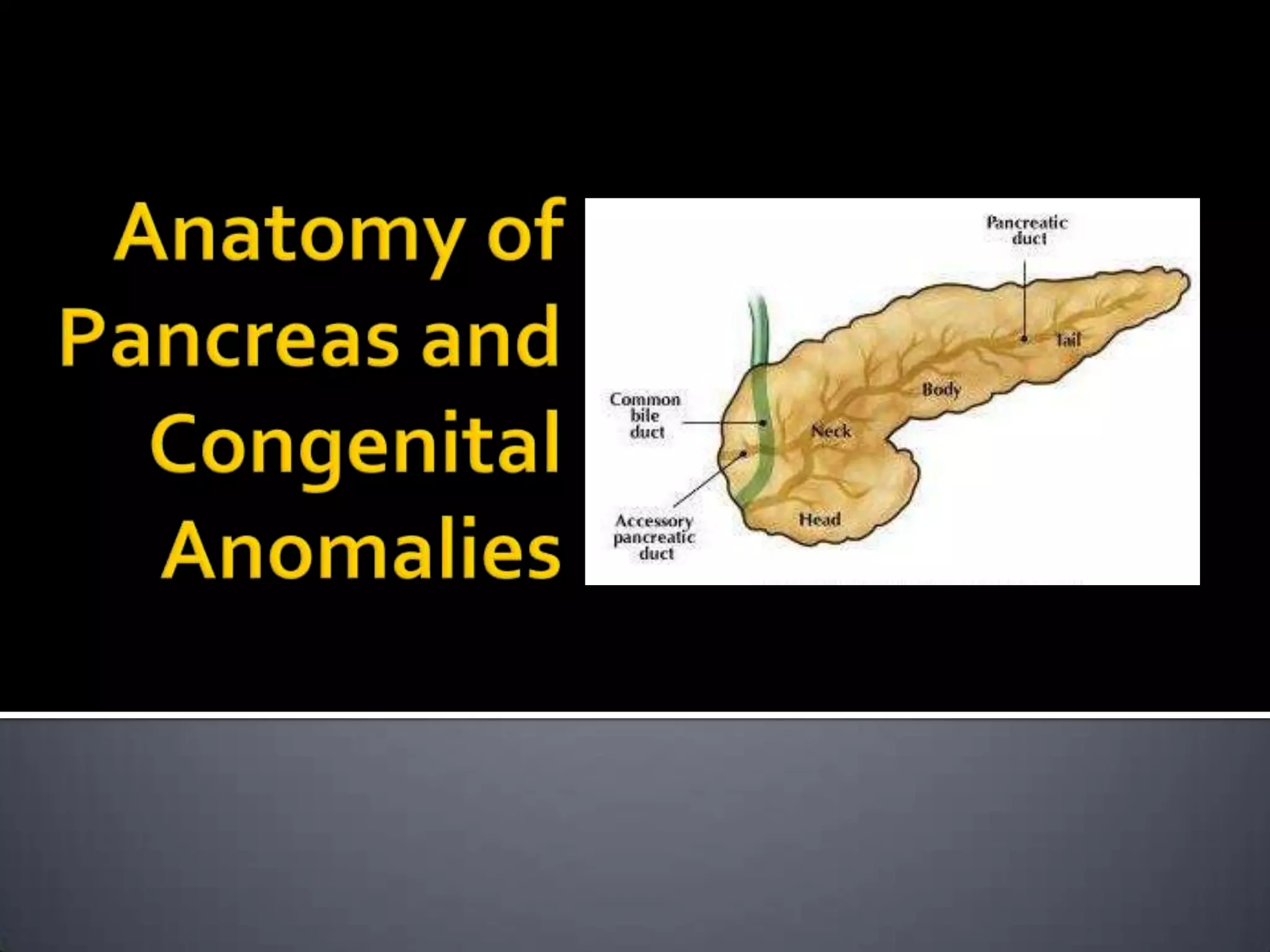
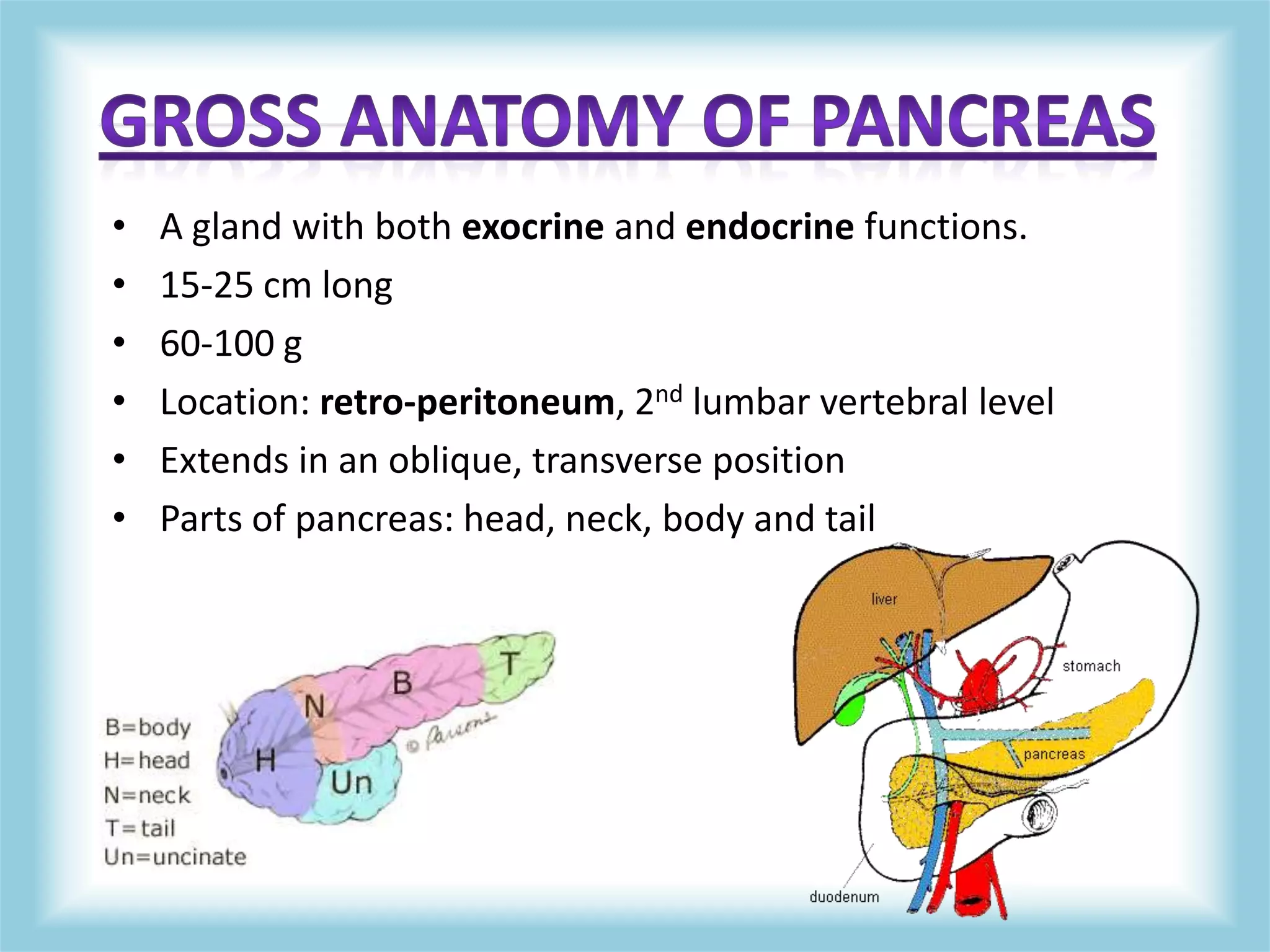
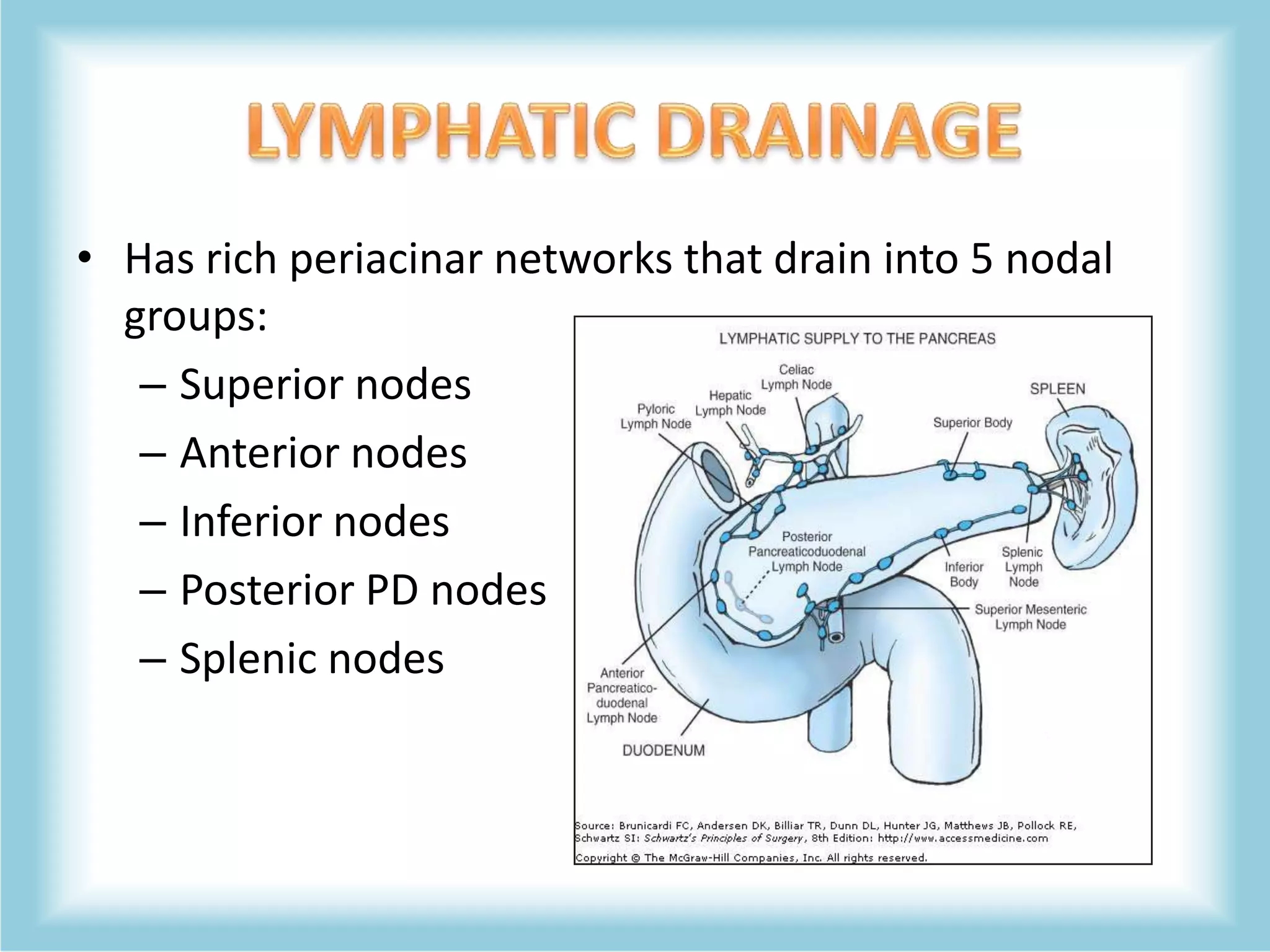
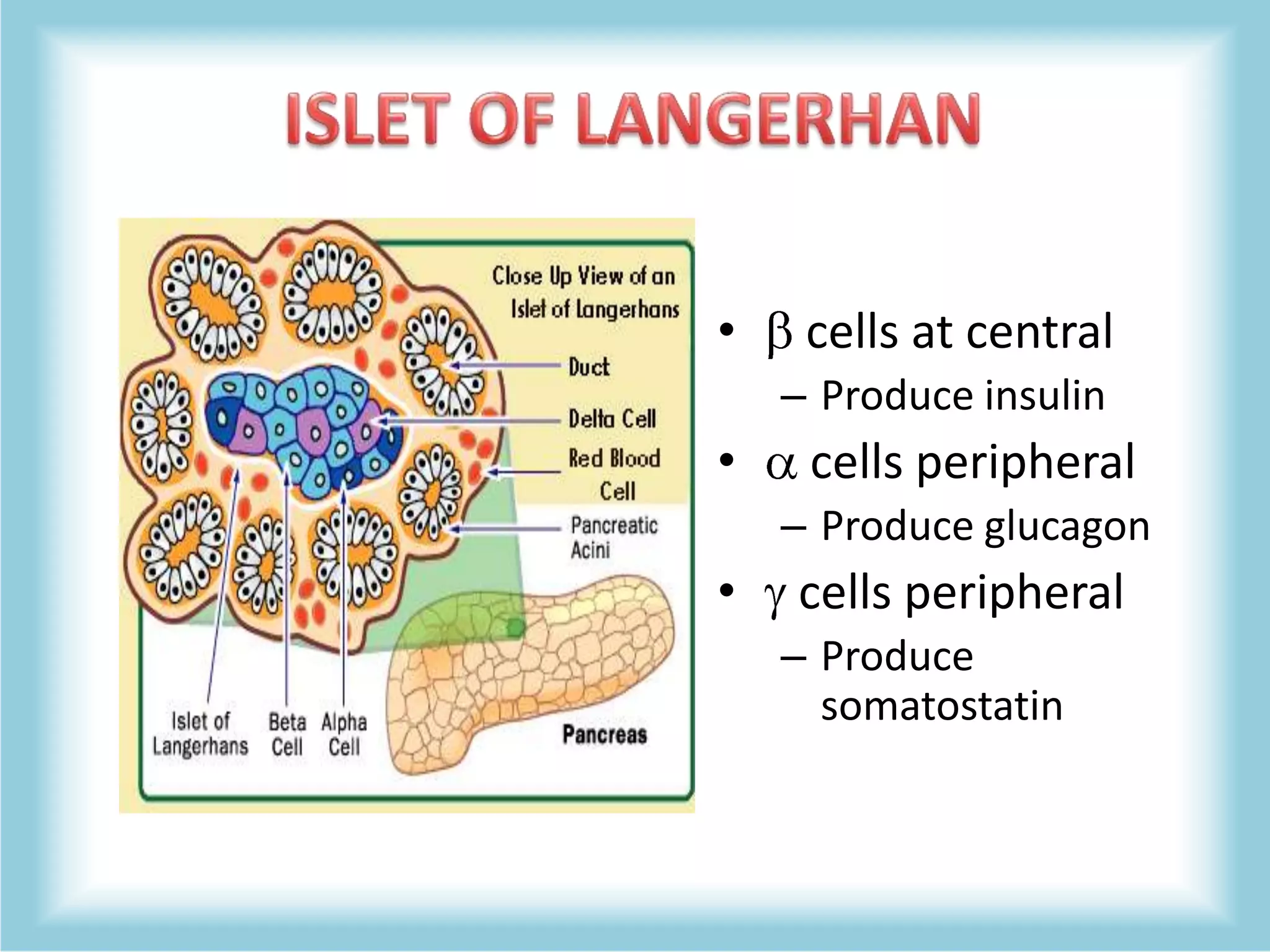
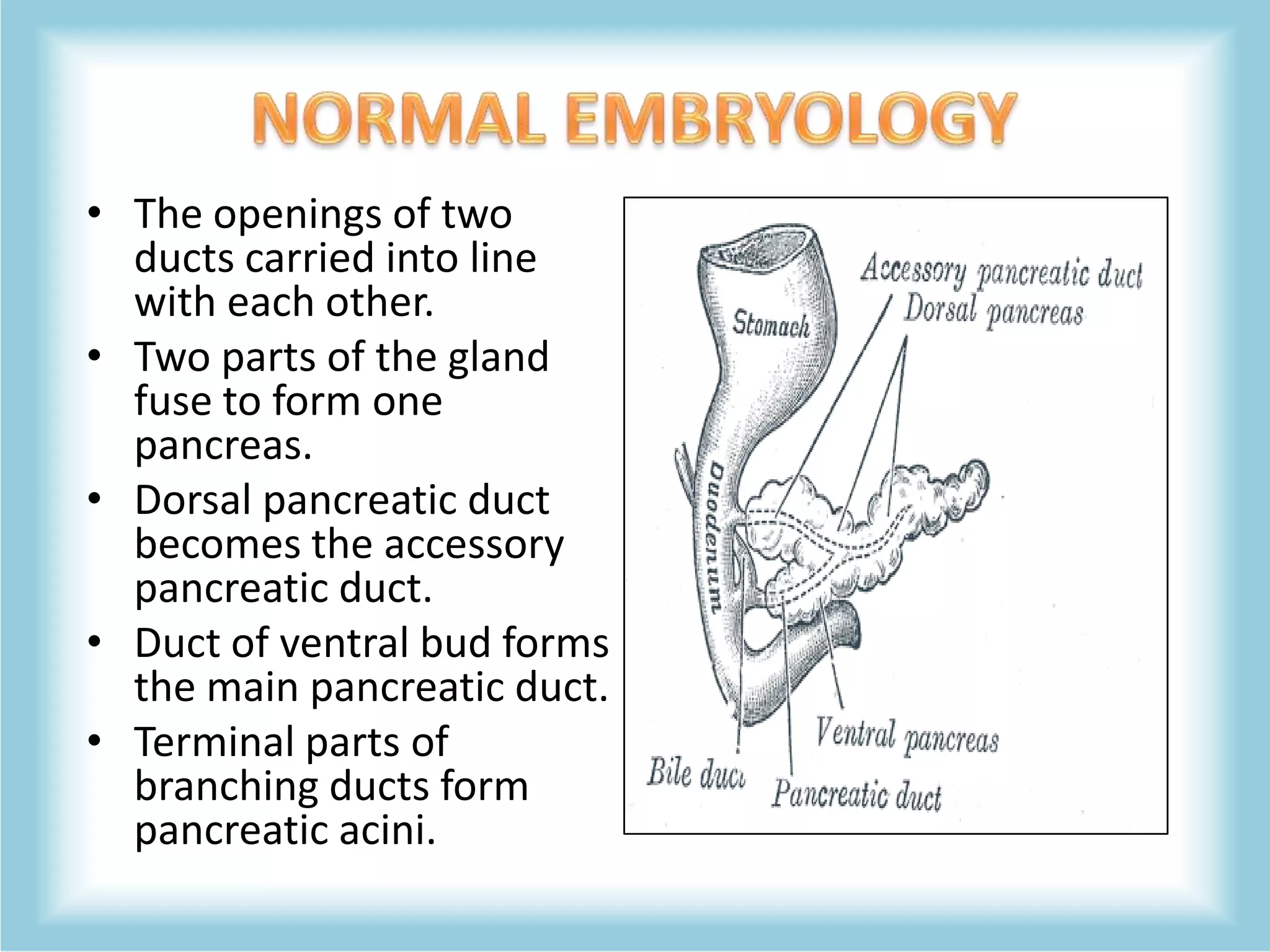
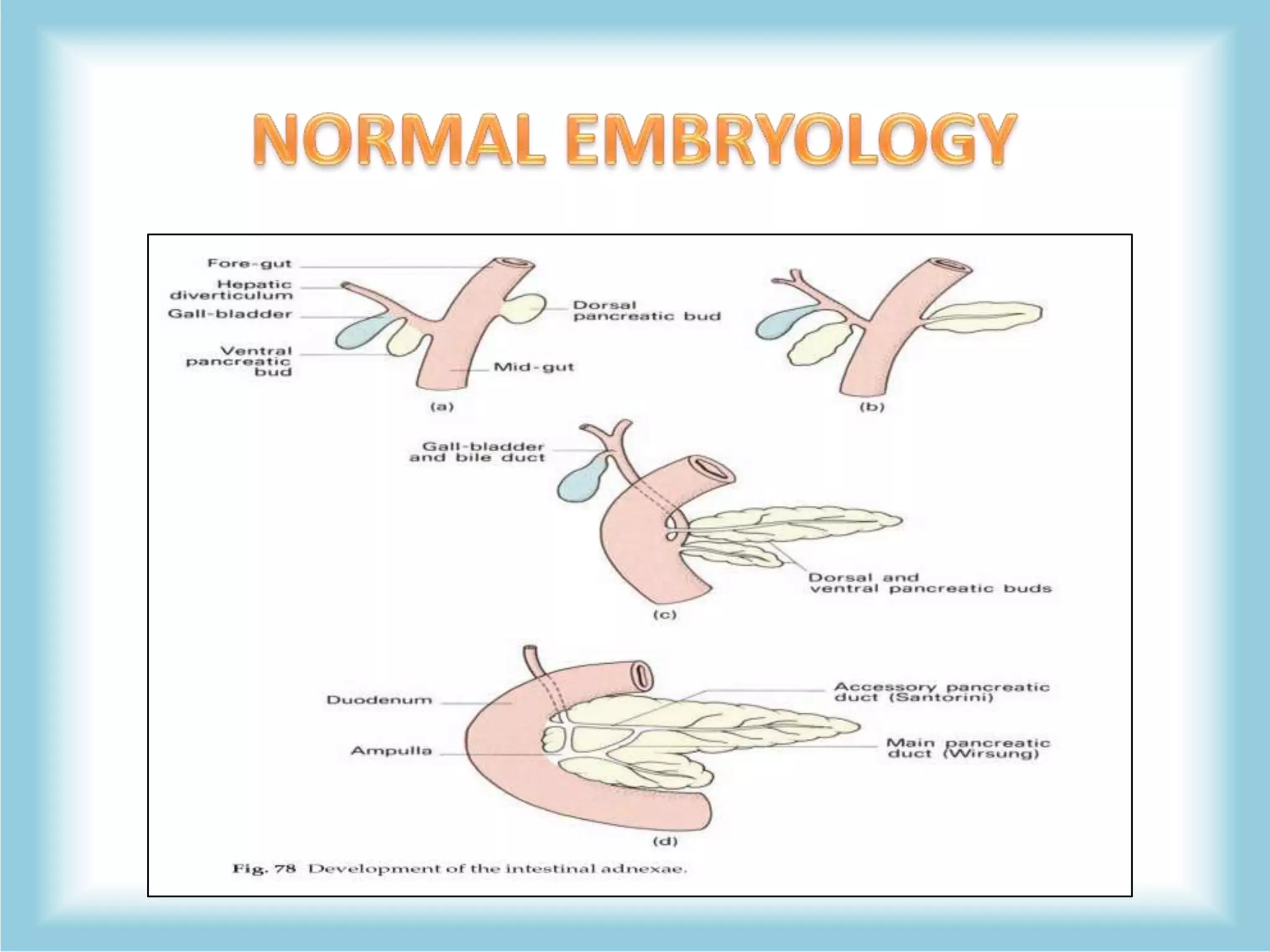
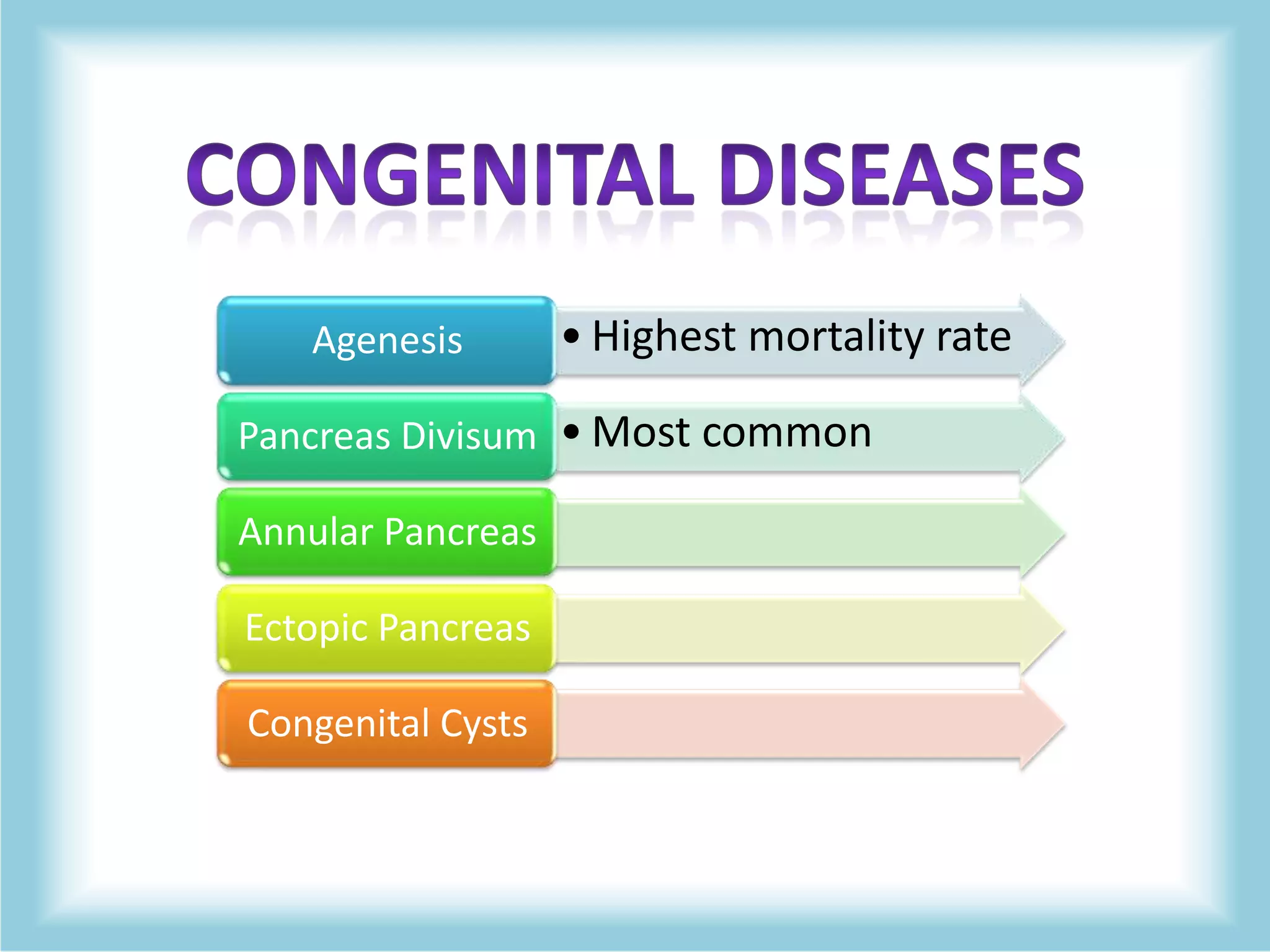
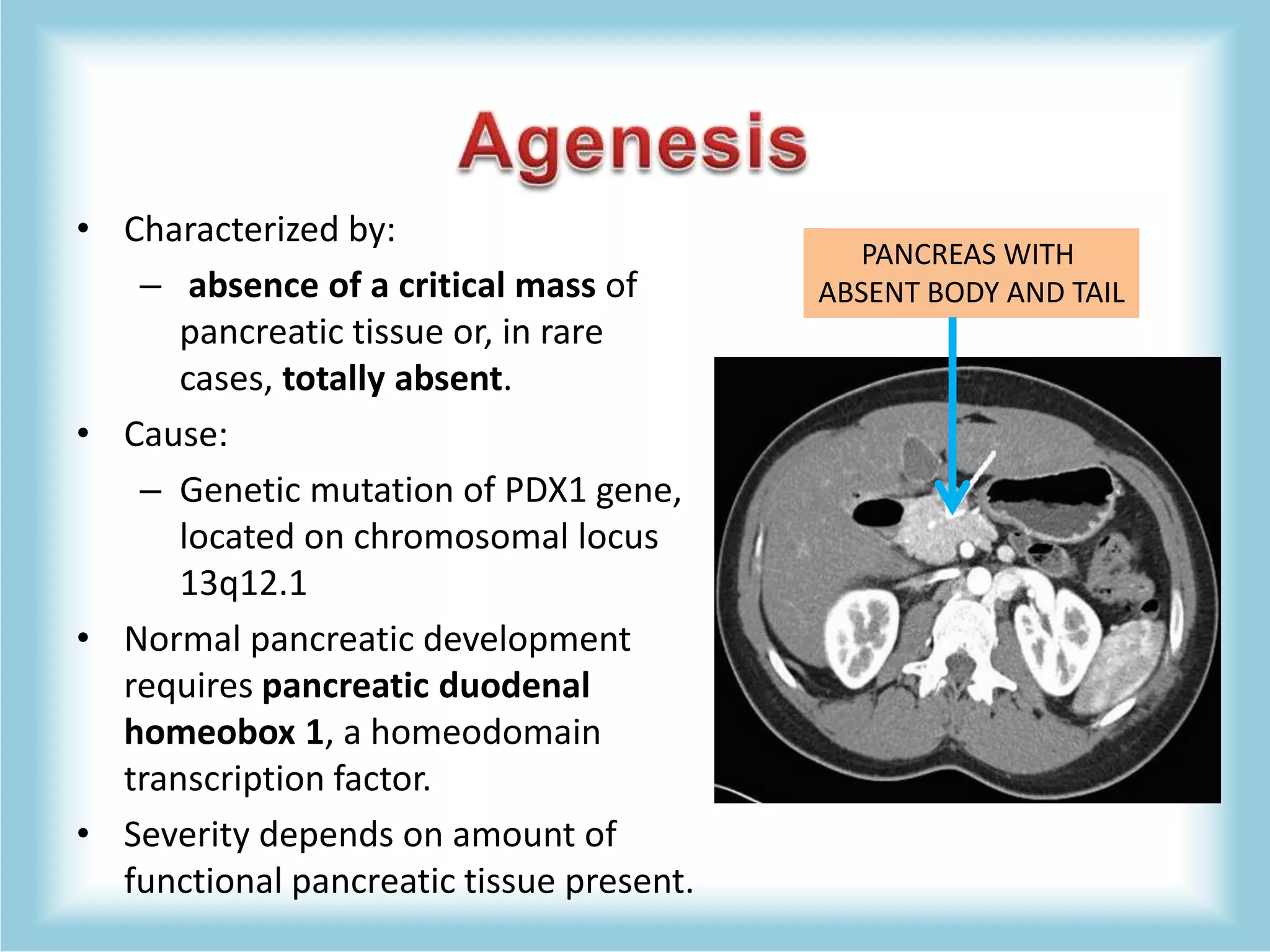
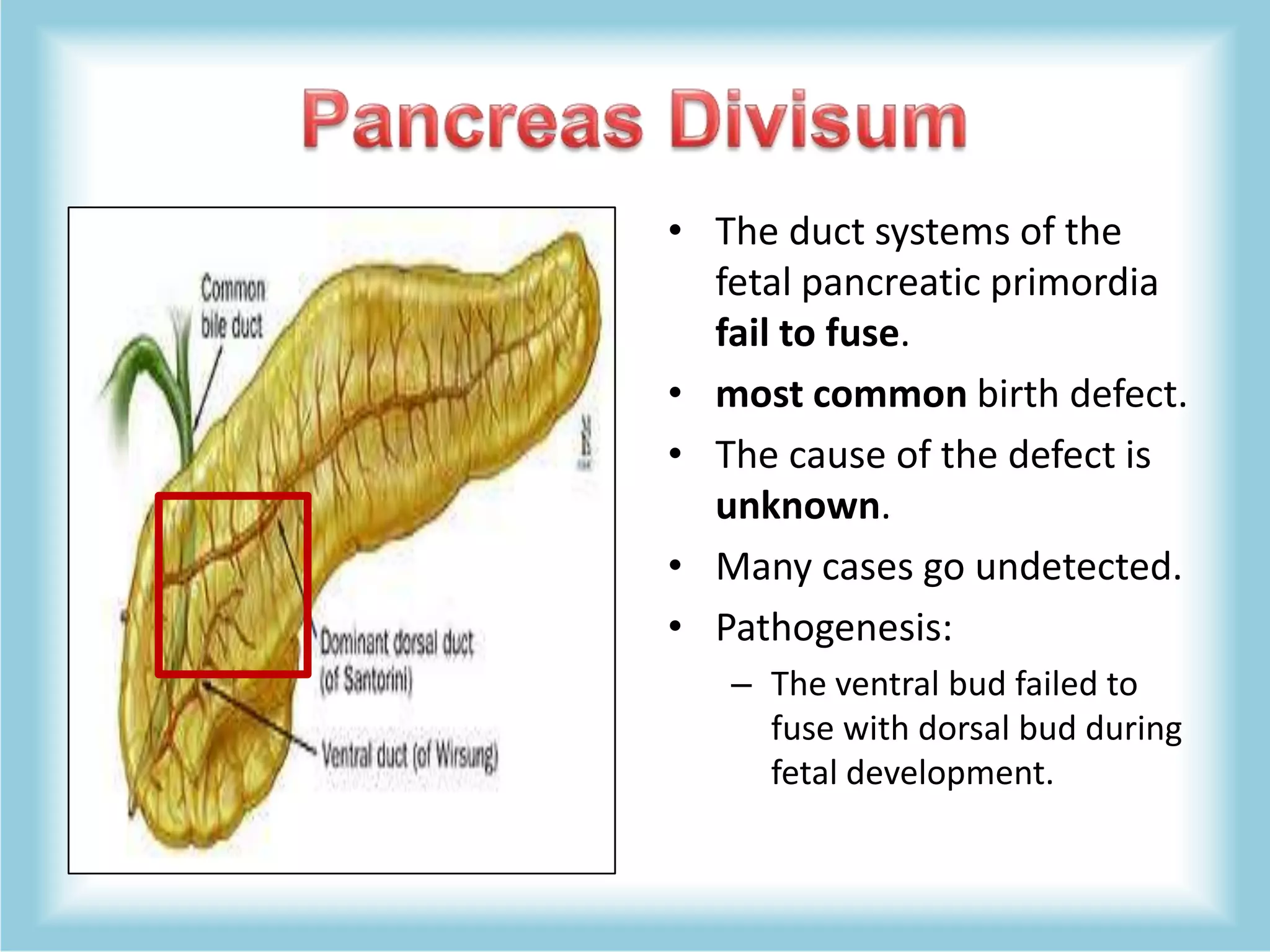
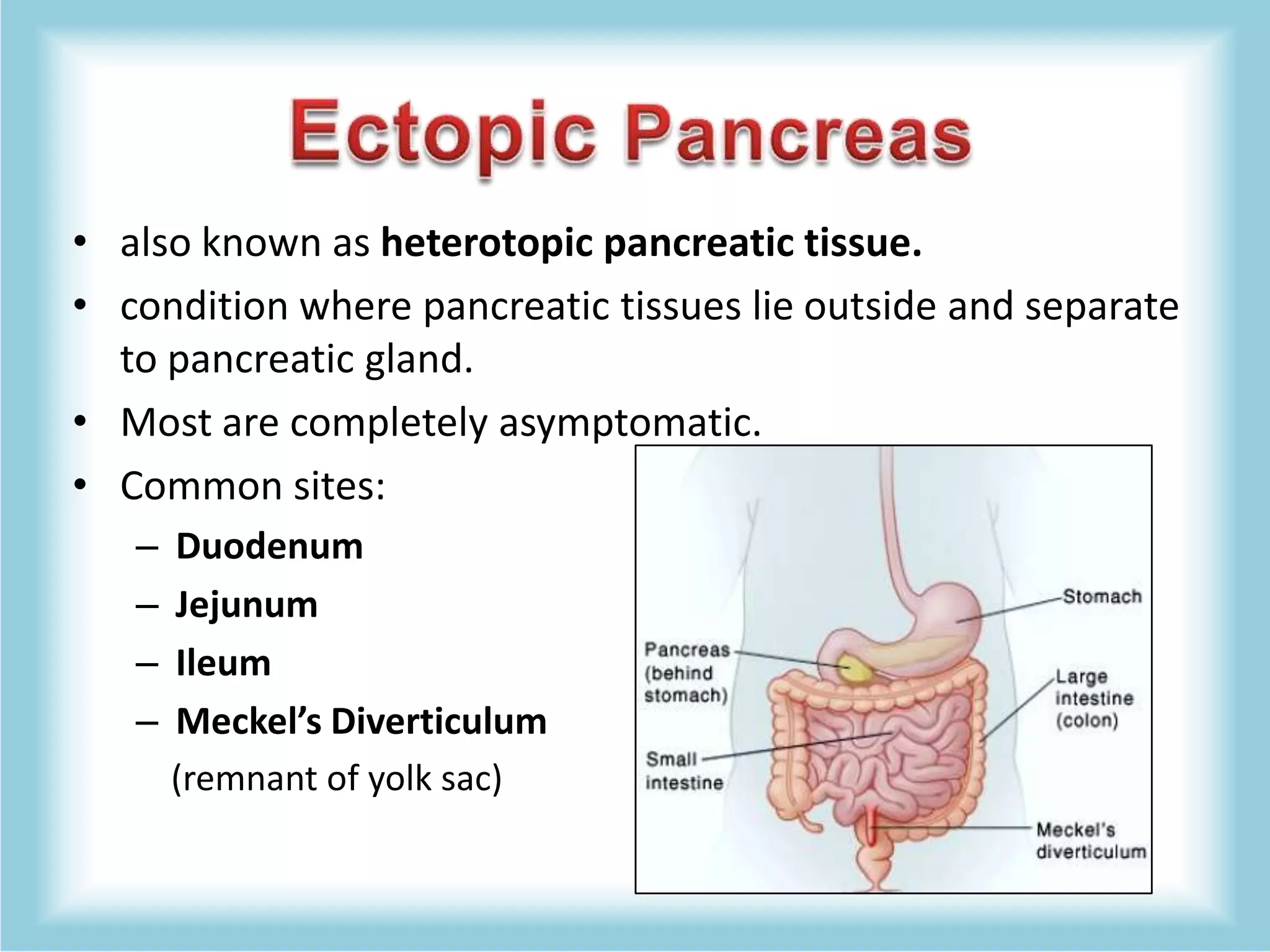
The document provides an overview of the anatomy, physiology, and congenital anomalies of the pancreas, detailing its structure, blood supply, and the types of congenital defects such as agenesis, pancreas divisum, annular pancreas, ectopic pancreas, and congenital cysts. It includes information on the exocrine and endocrine functions of the pancreas, the implications of pancreatic defects, and management strategies for associated conditions. The text also mentions the relevance of various diagnostic tests and the outcomes of surgical interventions.