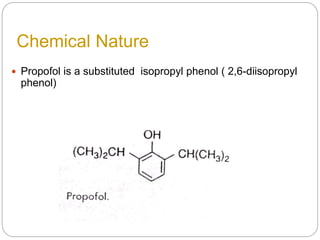
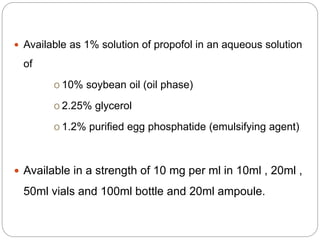
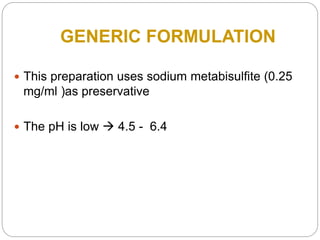
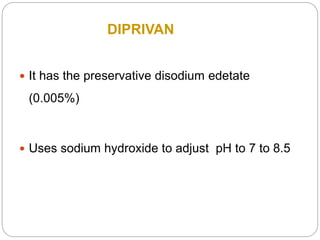
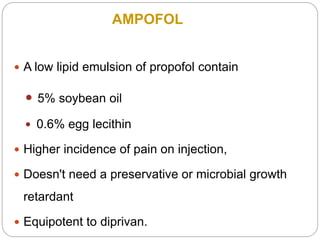
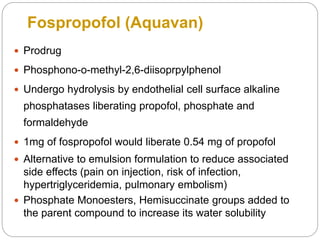
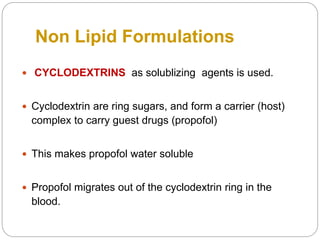
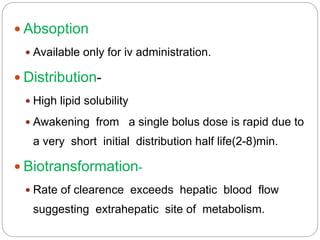
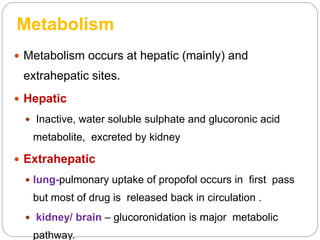
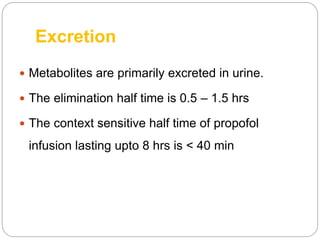
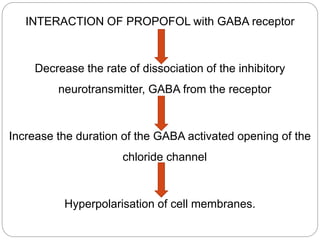
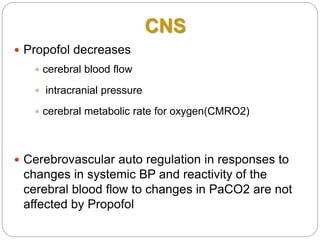
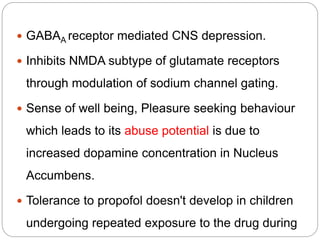
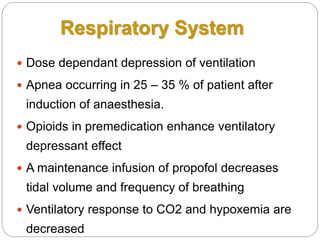
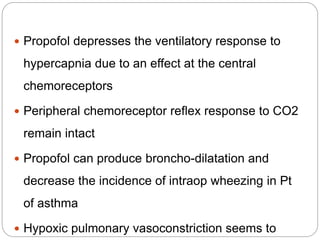
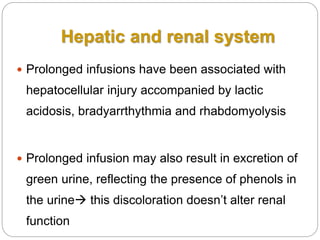
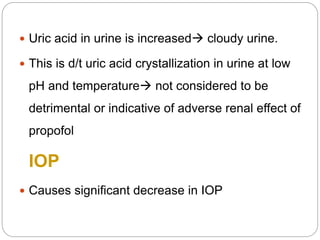
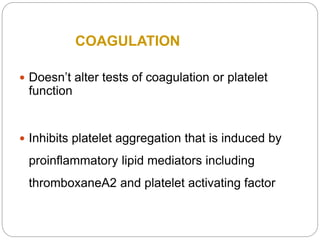
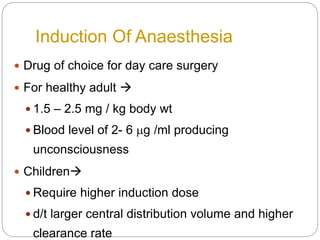
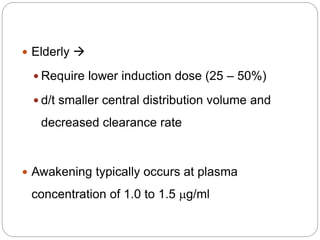
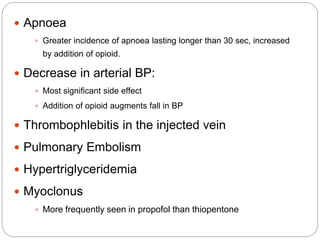
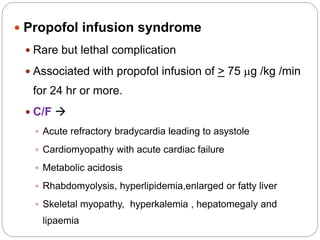
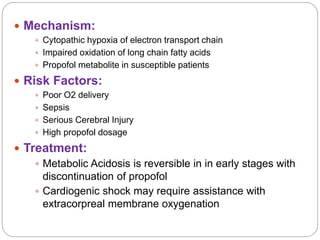
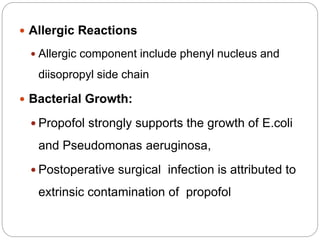
This document provides information on propofol, an intravenous anesthetic. It discusses propofol's history, chemical properties, formulations, pharmacokinetics, mechanisms of action, effects on organ systems, uses, adverse effects, and interactions. Propofol is a widely used anesthetic due to its rapid onset and offset of action. It acts by potentiating GABA receptors in the brain and has numerous clinical applications beyond general anesthesia induction. The document provides detailed information on propofol's properties and clinical use.