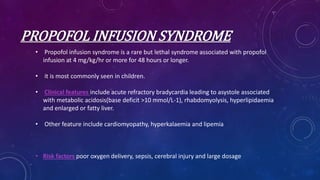
Intravenous anesthetics are fast-acting agents used for sedation and induction, with propofol being the most common due to its properties and pharmacokinetics. Ketamine offers dissociative anesthesia and is effective in cardiovascular patients, while midazolam is favored for its stability and utility in critical care settings. The document discusses the mechanisms, benefits, and side effects of these anesthetics, alongside dosage recommendations for various applications.