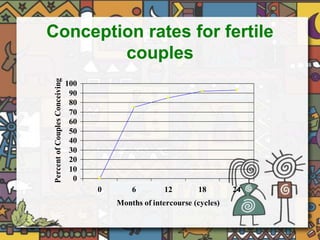
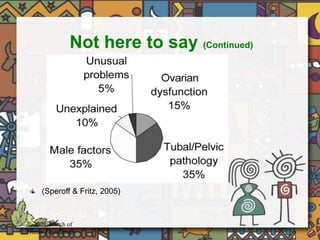
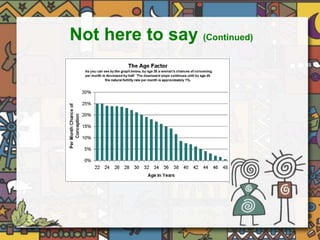
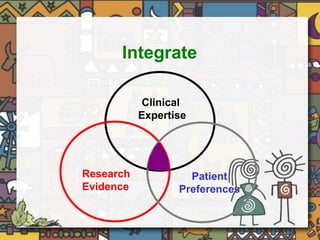
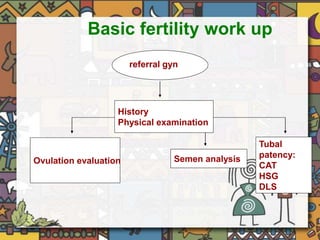
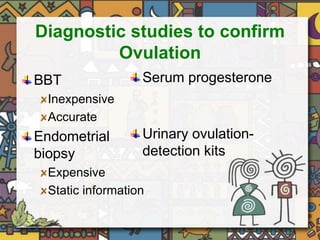
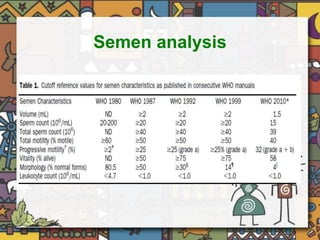
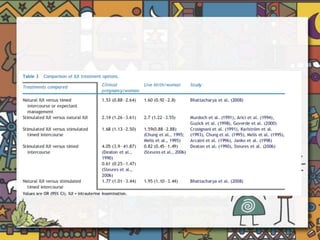
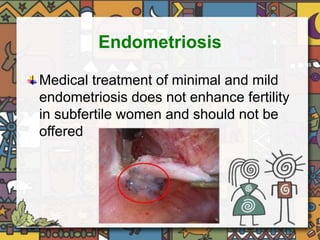
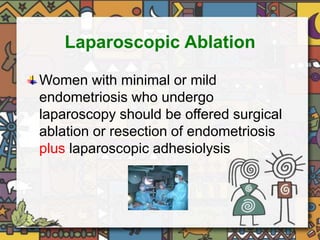
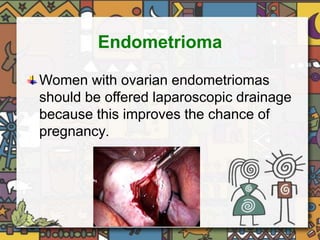
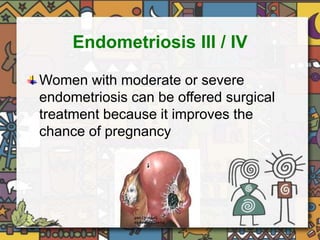
The document outlines evidence-based guidelines for the assessment and management of infertility, emphasizing the importance of integrating clinical expertise and patient preferences. It reviews various fertility treatments, investigations, and their efficacy, including recommendations against routine tests like post-coital tests, and the benefits of laparoscopic procedures for certain conditions. Key findings include treatment recommendations for conditions like PCOS, endometriosis, and the management of male factor infertility, highlighting the relevance of BMI and embryo transfer techniques in assisted reproduction success.