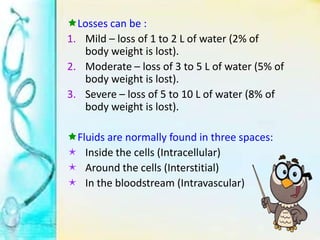
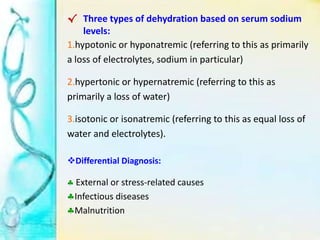
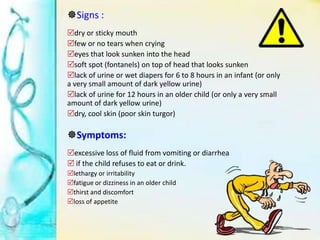
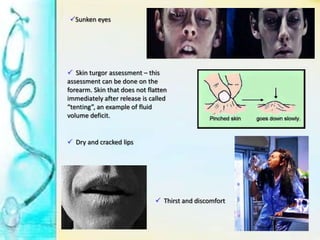
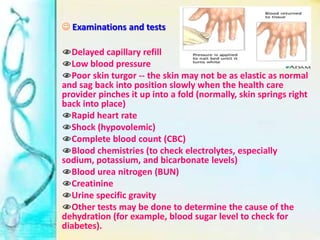
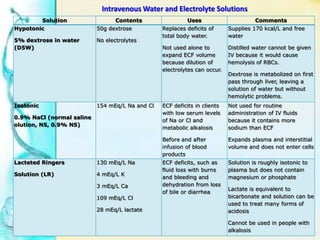
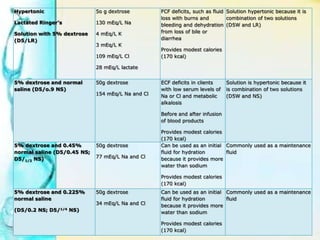
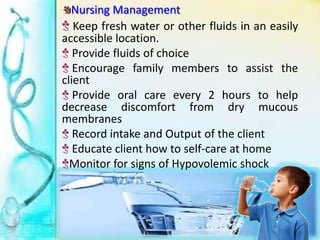
Dehydration occurs when the body loses more water and electrolytes than are taken in, usually through vomiting, diarrhea, excessive sweating, or inadequate fluid intake. It can range from mild to severe. Mild dehydration involves a 1-2% loss of body weight, while severe dehydration is a weight loss of 8% or more and involves electrolyte imbalances. Symptoms include thirst, lethargy, sunken eyes, and decreased skin elasticity. Treatment focuses on oral or IV fluid replacement depending on severity to replace fluid and electrolyte losses. Complications can include shock, seizures or brain damage if severe dehydration is left untreated.