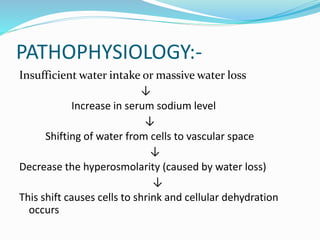
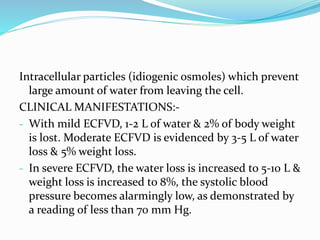
This document discusses extracellular fluid volume deficit (ECFVD), which is a decrease in intravascular and interstitial fluids that can lead to hypovolemia. There are two types of ECFVD: hyperosmolar, where fluid loss is greater than sodium loss, and iso-osmolar, where fluid and sodium are lost equally. ECFVD is caused by vomiting, diarrhea, blood loss, or fluid shifts. Symptoms include thirst, decreased skin turgor, dry mouth, low blood pressure, and tachycardia. Treatment involves oral or IV fluid replacement based on the severity of fluid loss to restore fluid balance and prevent complications like shock. Nursing care focuses on monitoring vital signs, fluid intake