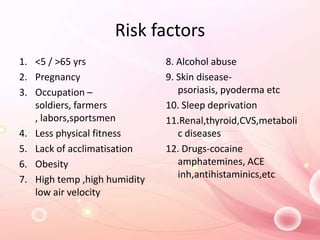
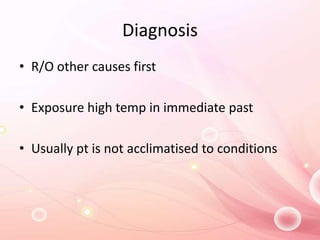
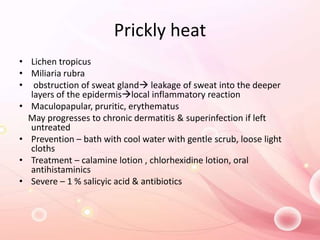
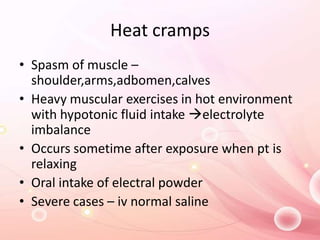
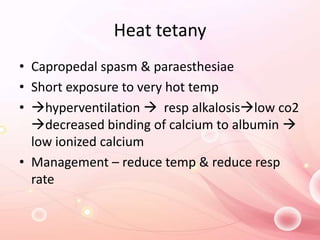
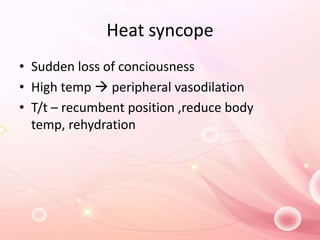
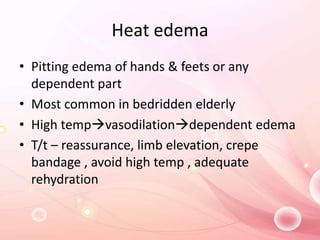
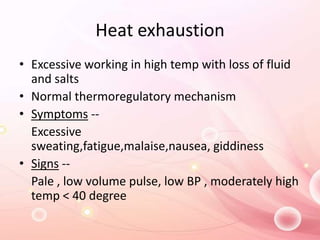
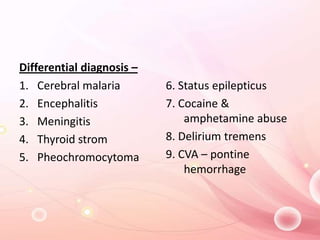
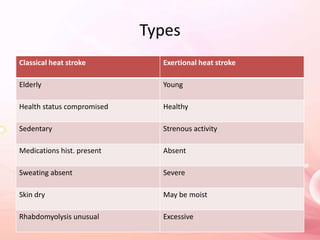
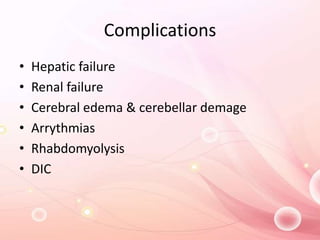
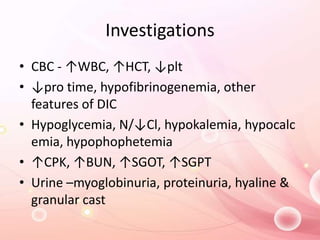
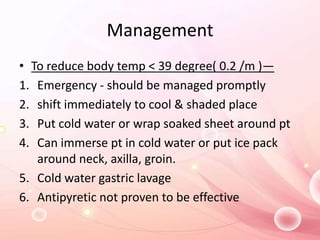
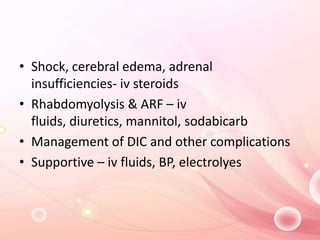
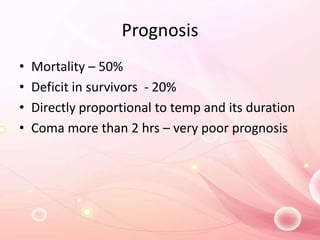
This document discusses heat stress and heat illness, including various conditions like prickly heat, heat cramps, heat tetany, heat syncope, heat edema, heat exhaustion, and heat stroke. It describes risk factors, symptoms, diagnosis, management, and prevention strategies for these conditions. The most severe form is heat stroke, which can be life-threatening and cause complications like hepatic or renal failure if not promptly treated by reducing core body temperature and providing supportive care. Prevention emphasizes adequate hydration, avoiding strenuous activity in high temperatures, and seeking medical help immediately if symptoms appear.