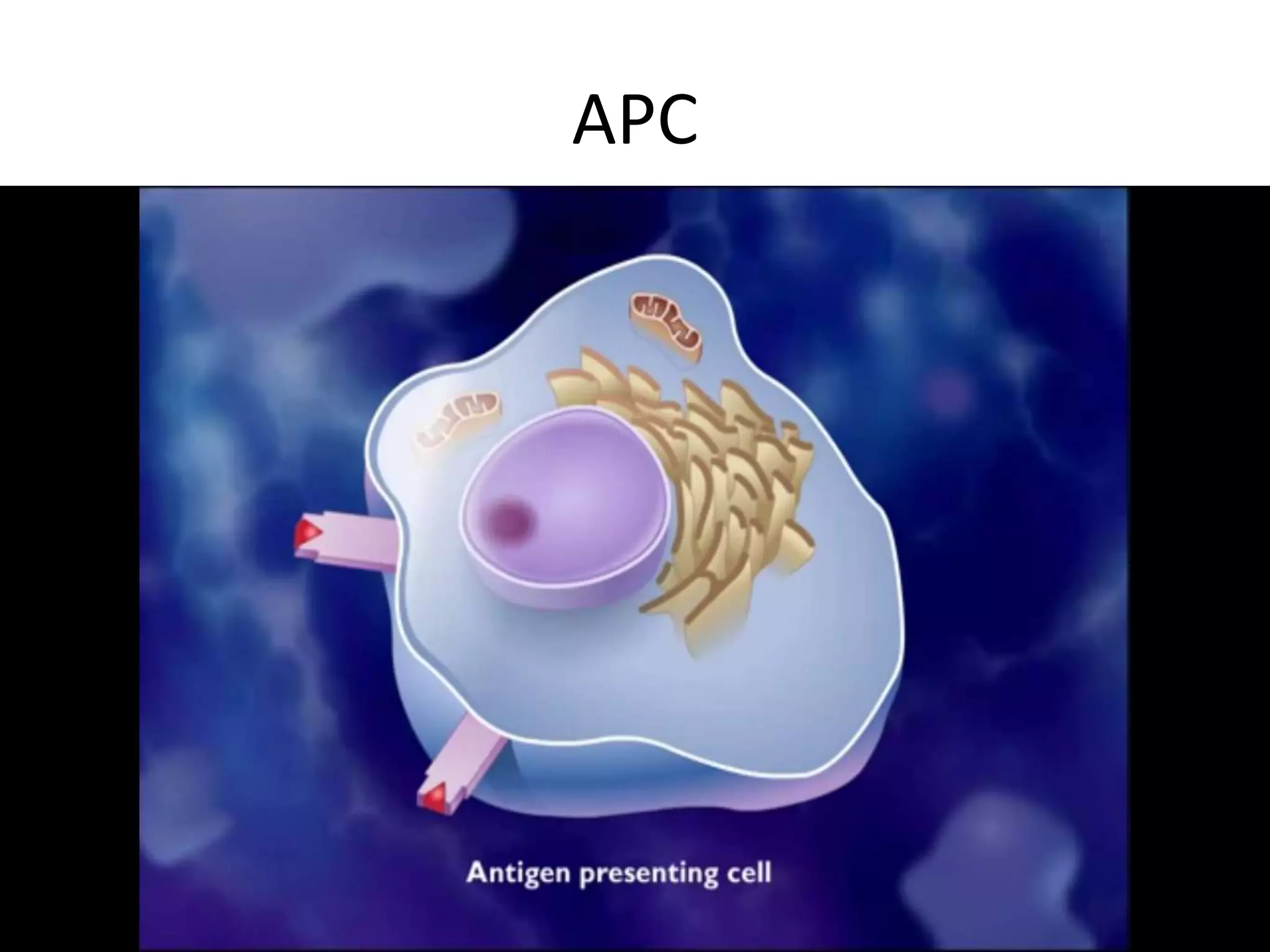
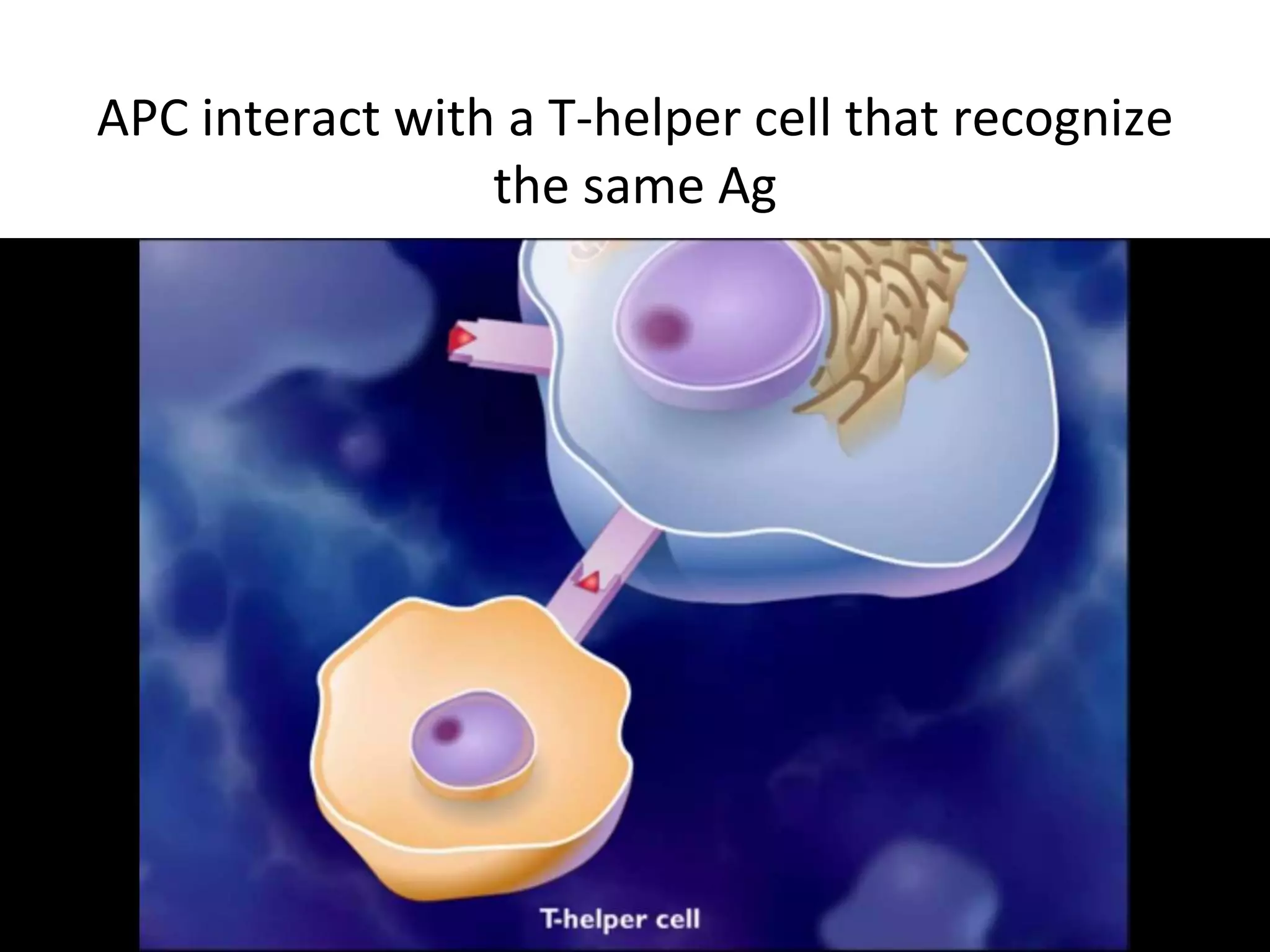
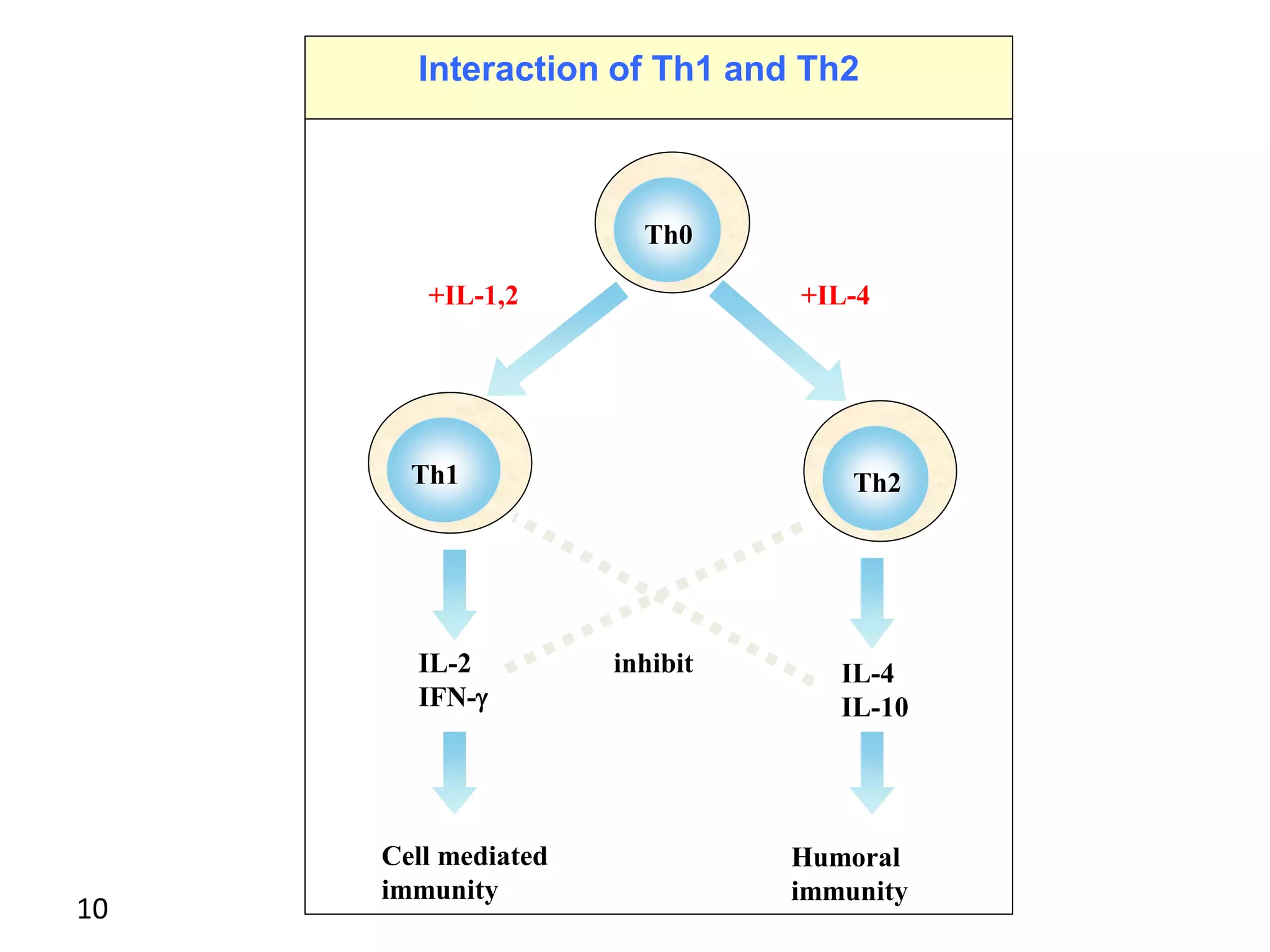
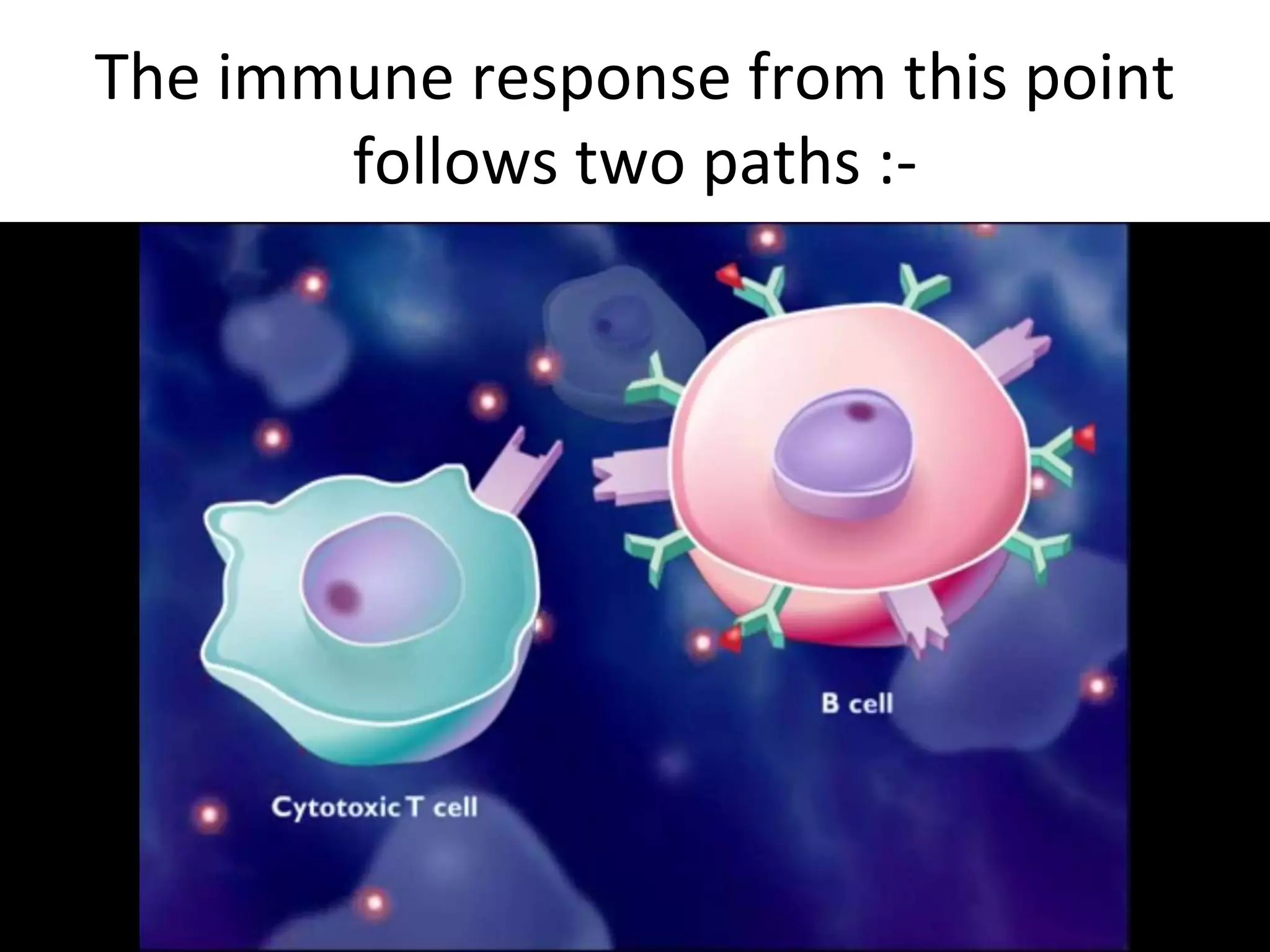
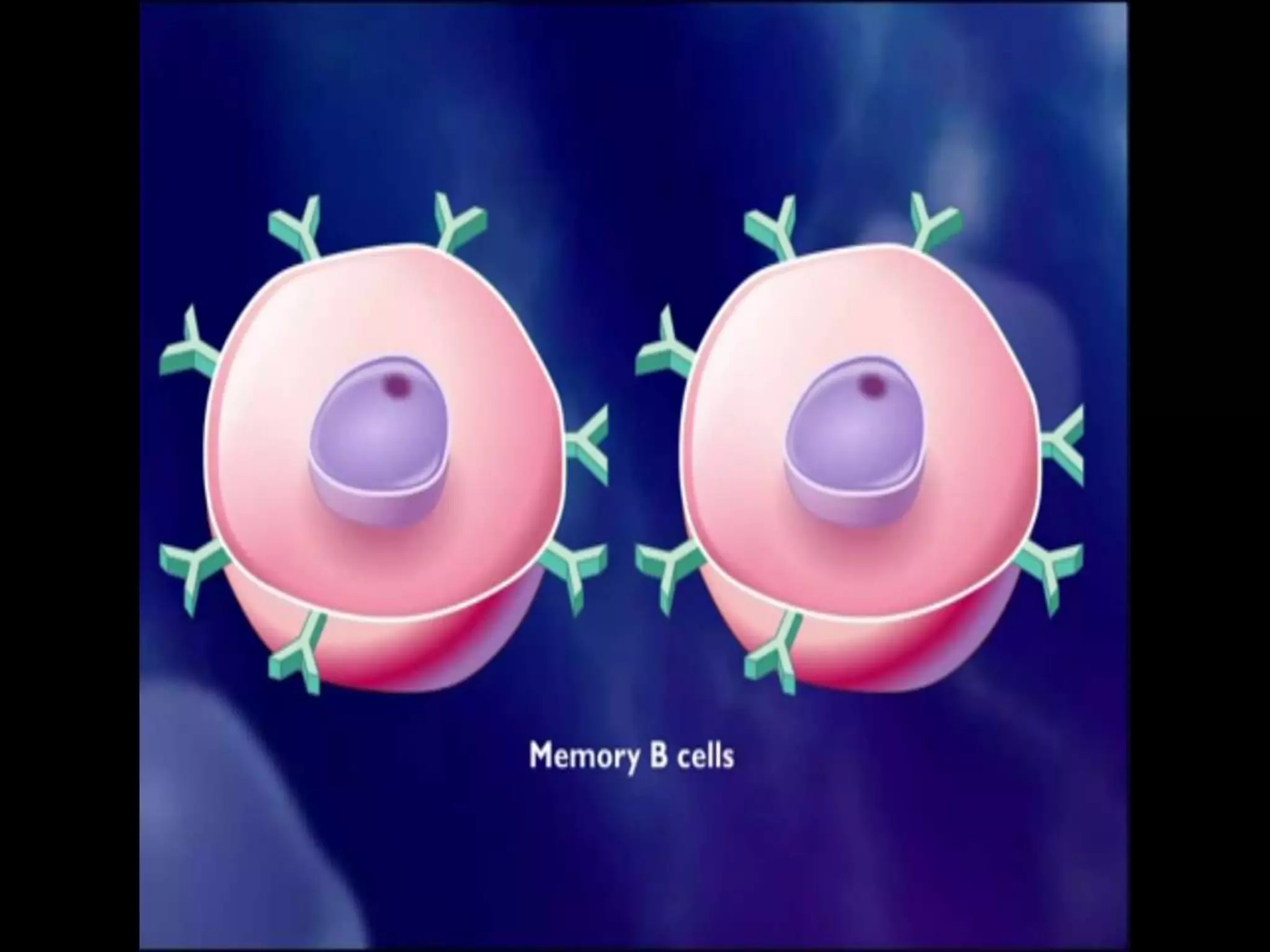
This document discusses immunoregulation and the various mechanisms that regulate immune responses. It describes how regulatory mechanisms act at all phases of the immune response, including recognition, activation, and effector function. Cytokines and regulatory T cells are highlighted as key regulators that can either stimulate or inhibit immune responses. The role of genetic factors in influencing immunoregulation is also summarized, noting genes related to immunoglobulins, T-cell receptors, and MHC complexes.