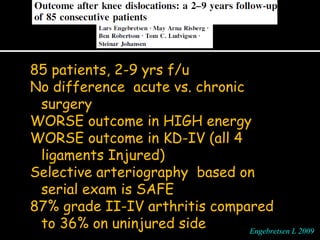
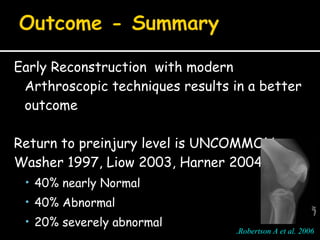
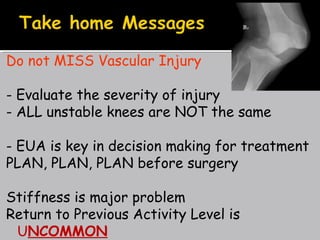
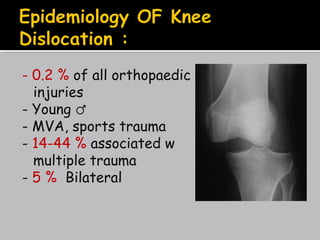
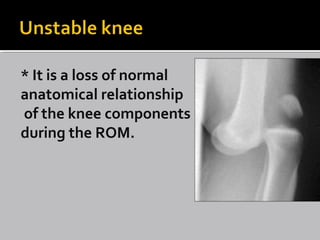
1. The document discusses knee dislocations, which occur when there is an abnormal relationship between the knee bones during range of motion.
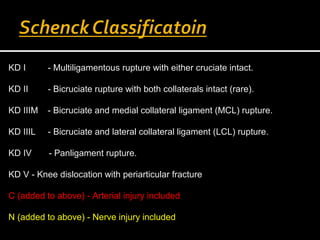
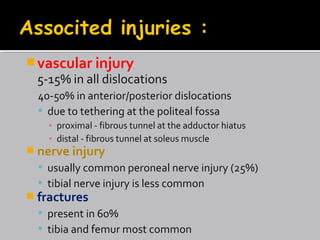
2. Knee dislocations are serious injuries that can impair physical activity and require evaluation of ligament injuries, fractures, arterial injuries and nerve injuries.
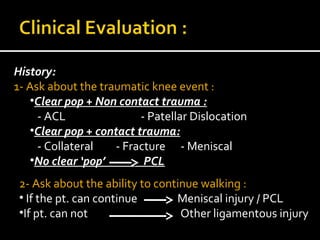
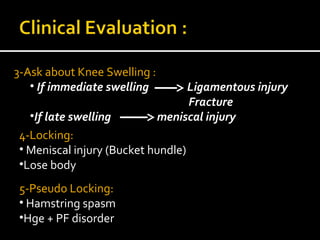
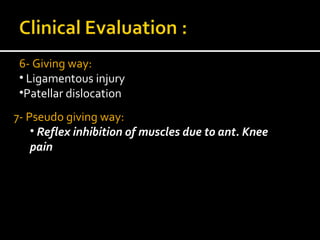
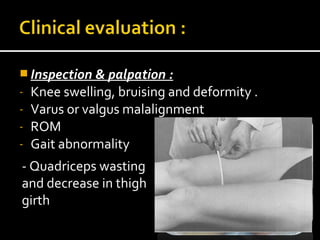
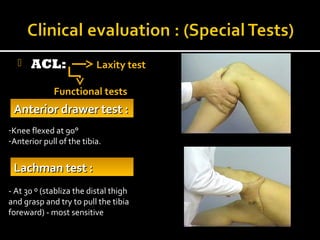
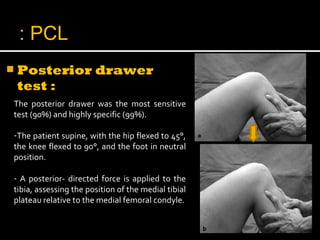
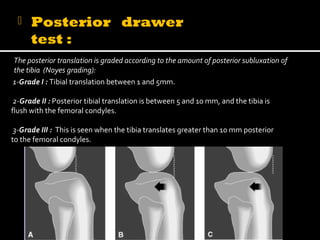
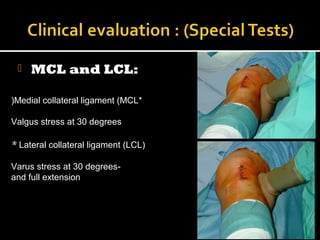
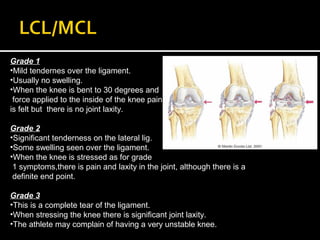
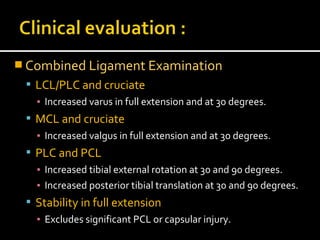
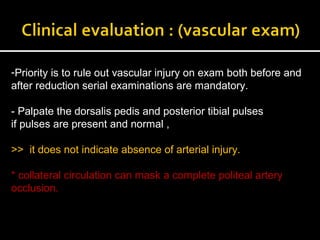
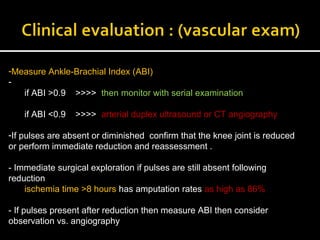
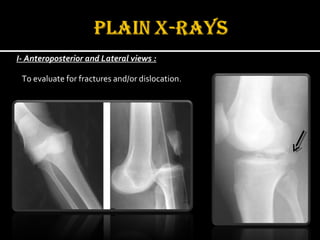
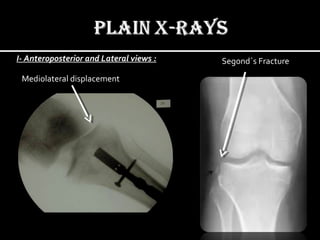
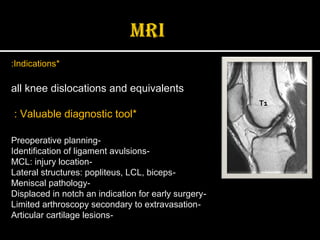
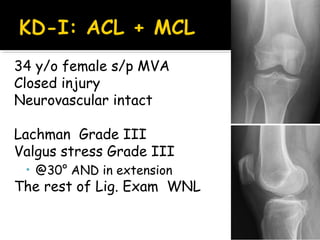
3. Evaluation involves physical examination of the knee ligaments using stress tests like anterior drawer, Lachman's and varus/valgus tests as well as imaging like x-rays and stress radiographs. Priority is given to evaluating for vascular injuries before and after reduction.
![Valgus + External Rotation is the
commonest medial side injury,
respectively;
1]. MCL then Medial capsule
2]. ACL
3]. MM = “O'DONOGHUE UNHAPPY
TRIAD”
Valgus + External Rotation is the
commonest medial side injury,
respectively;
1]. MCL then Medial capsule
2]. ACL
3]. MM = “O'DONOGHUE UNHAPPY
TRIAD”
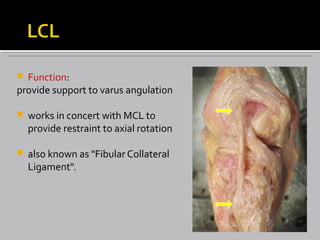
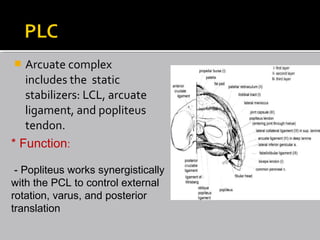
Varus + Internal injury of lat ligaments of
the knee;
1]. LCL then lateral capsule
2]. ACL
3]. Arcuate complex
4]. Popliteus tendon
5]. ITB
6]. Biceps femoris
7]. Common peroneal nerve,
Varus + Internal injury of lat ligaments of
the knee;
1]. LCL then lateral capsule
2]. ACL
3]. Arcuate complex
4]. Popliteus tendon
5]. ITB
6]. Biceps femoris
7]. Common peroneal nerve,](https://image.slidesharecdn.com/activitypresentation-160221172004/85/KNEE-INJURIES-19-320.jpg)
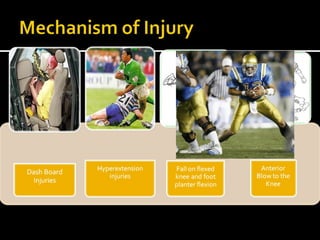
![HYPEREXTENSION mechanism:
1]. ACL
2]. PCL & posterior capsule
HYPEREXTENSION mechanism:
1]. ACL
2]. PCL & posterior capsule
• ANTERO-POSTERIOR
DISPLACEMENT: e.g. dashboard
accident:
1]. ACL or
2]. PCL
• ANTERO-POSTERIOR
DISPLACEMENT: e.g. dashboard
accident:
1]. ACL or
2]. PCL](https://image.slidesharecdn.com/activitypresentation-160221172004/85/KNEE-INJURIES-20-320.jpg)