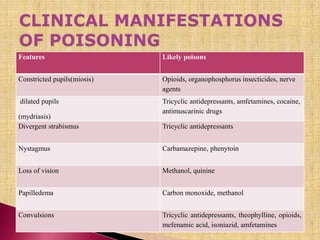
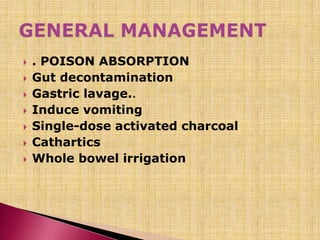
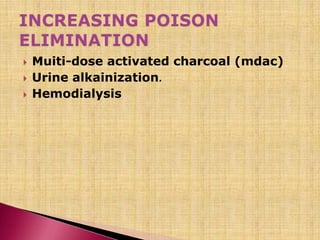
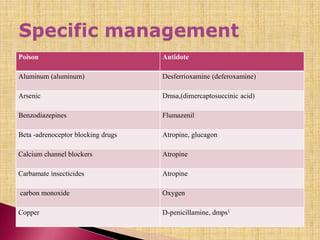
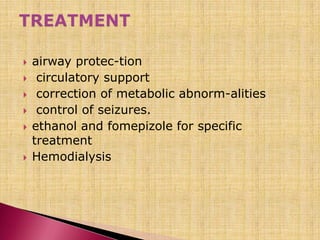
A poison is any substance that causes harm if it gets into the body in large enough doses. The amount of a substance that enters the body is called the dose. Poisons can enter the body through ingestion, inhalation, skin contact, or injection. Common poisons include drugs, household chemicals, pesticides, carbon monoxide, and snake venom. Symptoms and treatment depend on the specific poison, but often involve supporting vital functions and detoxification through methods like activated charcoal or dialysis.






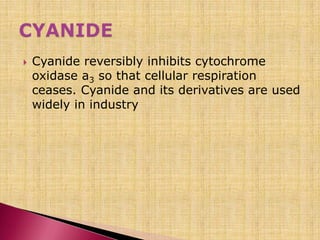





![ The methylxanthines theobromine and
caffeine can be found in a variety of
substances (e.g., chocolate, cocoaand
coffee beans, over-the-countersleep
prevention aids, asthma medications
[theophylline, aminophylline]).](https://image.slidesharecdn.com/poisoningtoxicology-140427003447-phpapp01/85/Poisoning-toxicology-77-320.jpg)