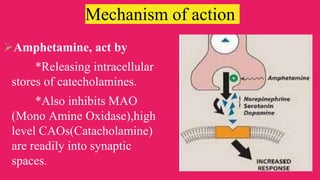
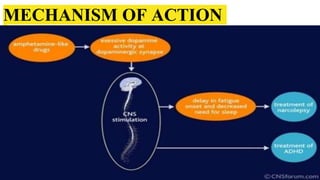
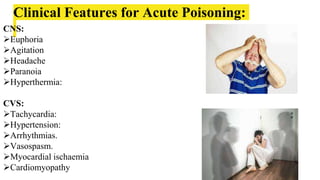
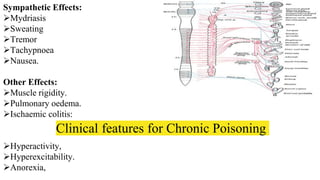
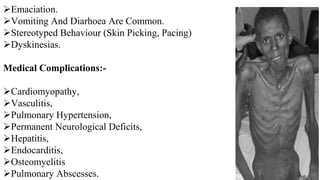
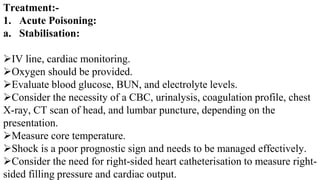
Amphetamine is a central nervous system stimulant associated with both therapeutic uses and potential for abuse, leading to toxicity. Symptoms of acute and chronic poisoning include agitation, hyperthermia, tachycardia, and cardiovascular complications. Treatment focuses on stabilization and supportive care; prevention strategies emphasize parental guidance and secure medication practices.

![Epidemiology:
The worldwide prevalence of amphetamine use is estimated to be 0.3%
to 1.1% as per the United Nations Office of Drugs and Crime data from
2013. Misuse of Amphetamine and METH has been increasing in the
United States as the hospital admissions increased by more than 500%
between 1992 and 2002. Men have a higher prevalence of amphetamine
misuse compared to women. The overall prevalence of amphetamine use
in the United States in individuals aged 12 or older was 4.7% in 2013 as
per the National Survey of Drug Use and Health.[5][5]](https://image.slidesharecdn.com/amphetaminetoxicityslideshare-210616134610/85/Amphetamine-toxicity-slideshare-11-320.jpg)
![v. Diazepam and chlorpromazine have been effective in
treating amphetamine-induced chorea.
vi. No specific antidotes for Amphetamine poisoning.
vii. The drugs like Imipramine and fluoxetine [adjuvent
pharmacological agents to treat the symptoms, but
results are disappointing.]
viii. Those with moderately dependence can be treated on an
Outpatient basis without using drugs.](https://image.slidesharecdn.com/amphetaminetoxicityslideshare-210616134610/85/Amphetamine-toxicity-slideshare-21-320.jpg)