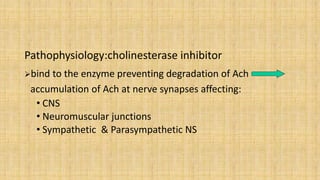
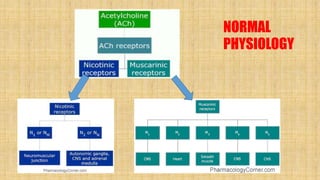
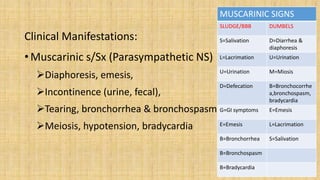
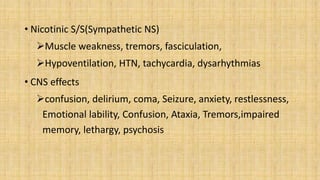
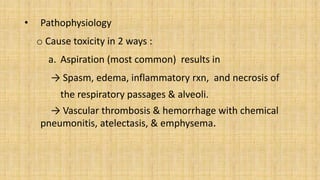
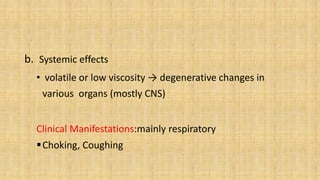
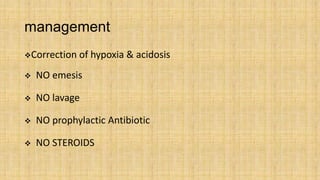
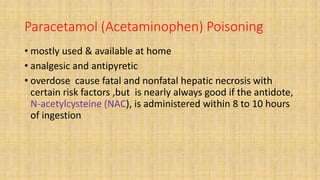
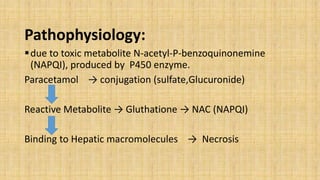
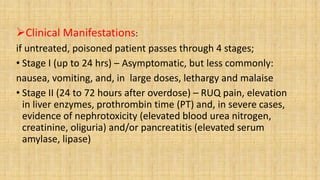
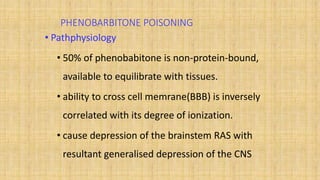
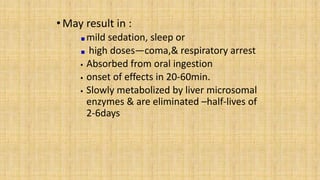
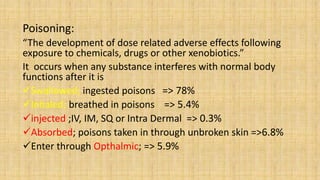
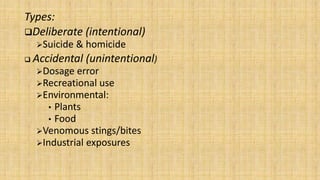
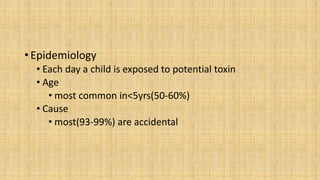
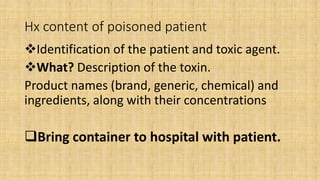
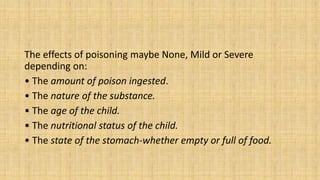
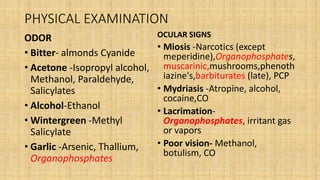
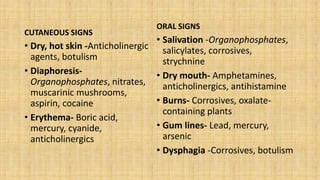
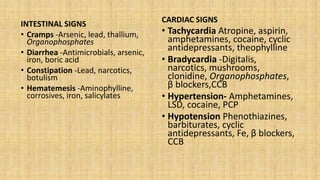
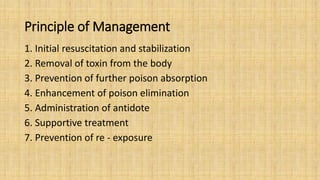
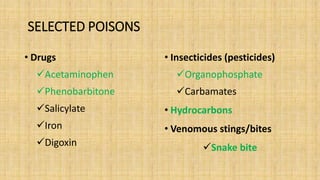
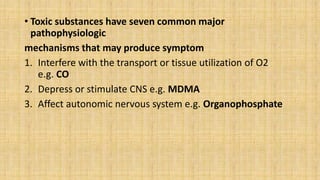
This document summarizes a seminar on poisoning that covered definitions, types, epidemiology, history and physical examination, clinical diagnosis, management principles, and some common poisonings. It defined poisoning as the development of adverse effects from exposure to chemicals, drugs, or other substances. The seminar outlined the epidemiology, types, clinical presentation, diagnostic workup, and management principles for poisonings. It also provided details on the pathophysiology, clinical manifestations, and treatment of specific poisonings including organophosphates, hydrocarbons, and paracetamol.

![Organophosphate poisoning
• Less common (< 1%) in children
• Mostly accidental and unintentional
• More common in lower socioeconomic class
• Used in agriculture(crop sprays) and home as insecticides &
pesticides
e.g.
Insecticides – malathion(MLT), parathion, ethion, diazinon
Nerve gases - sarin, tabun
ophthalmic agents - echothiophate, isoflurophate
Herbicides - tributes [DEF], merphos](https://image.slidesharecdn.com/seminaronpoisoning-180511093355/85/Seminar-on-poisoning-25-320.jpg)