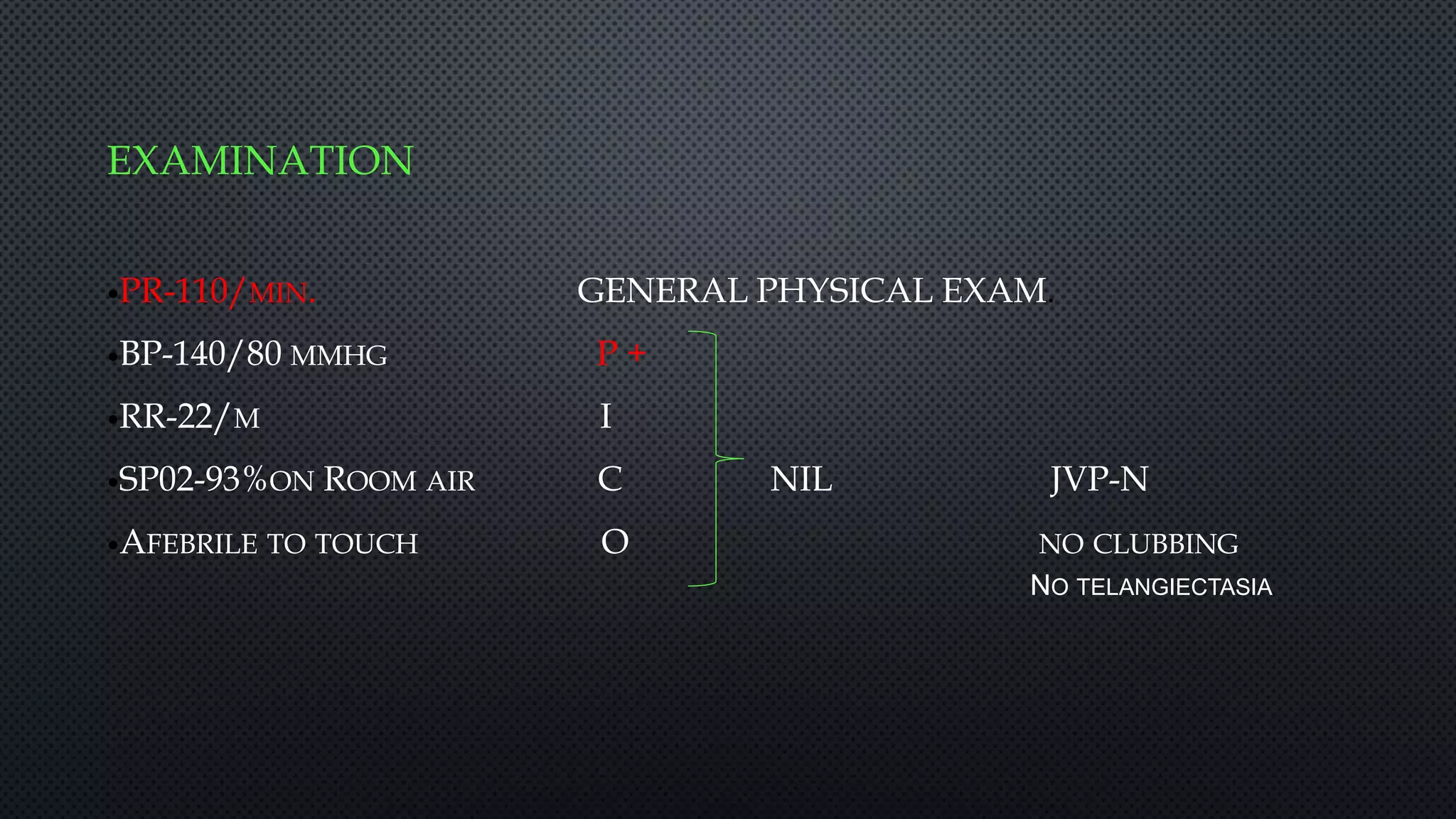
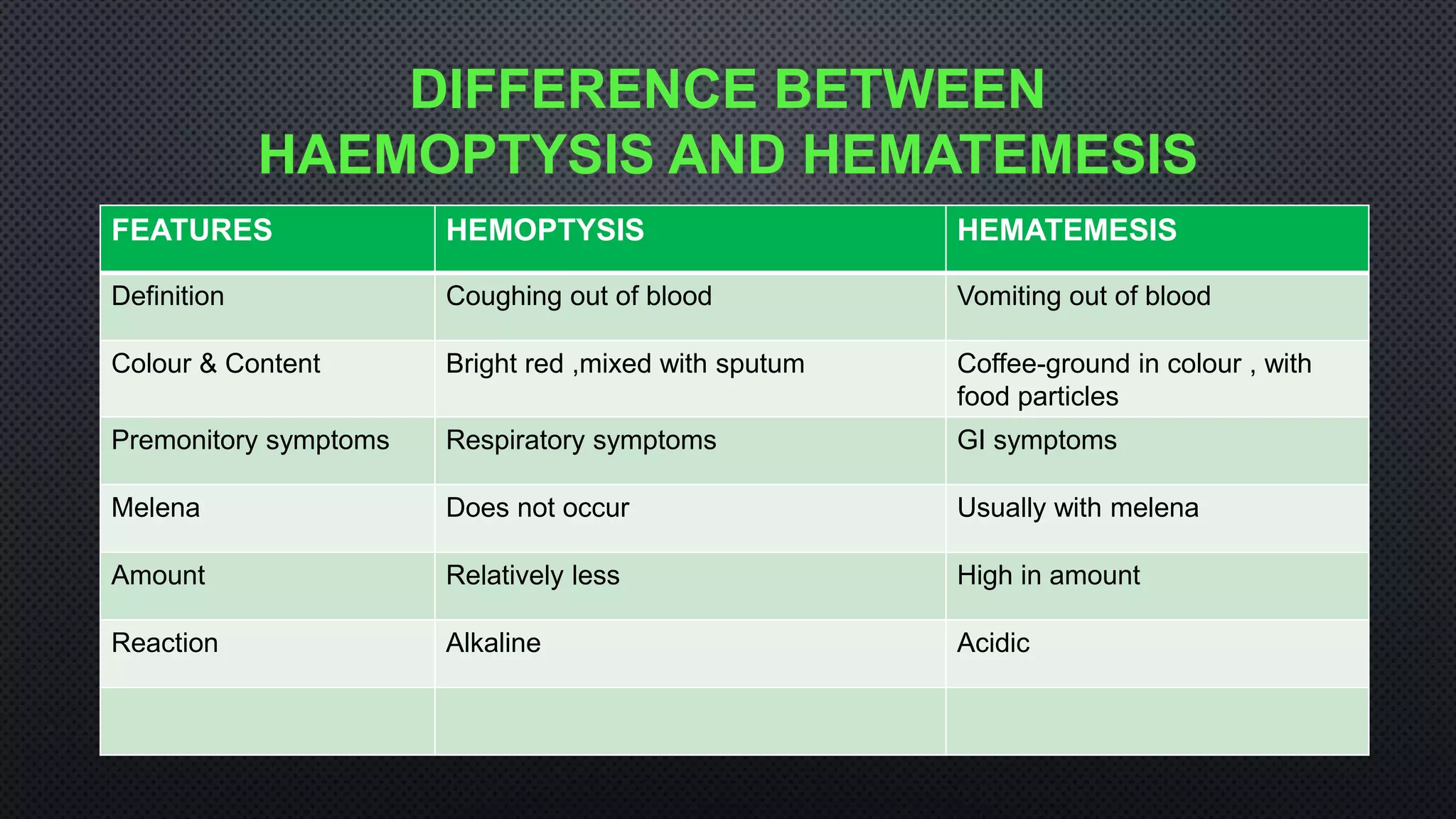
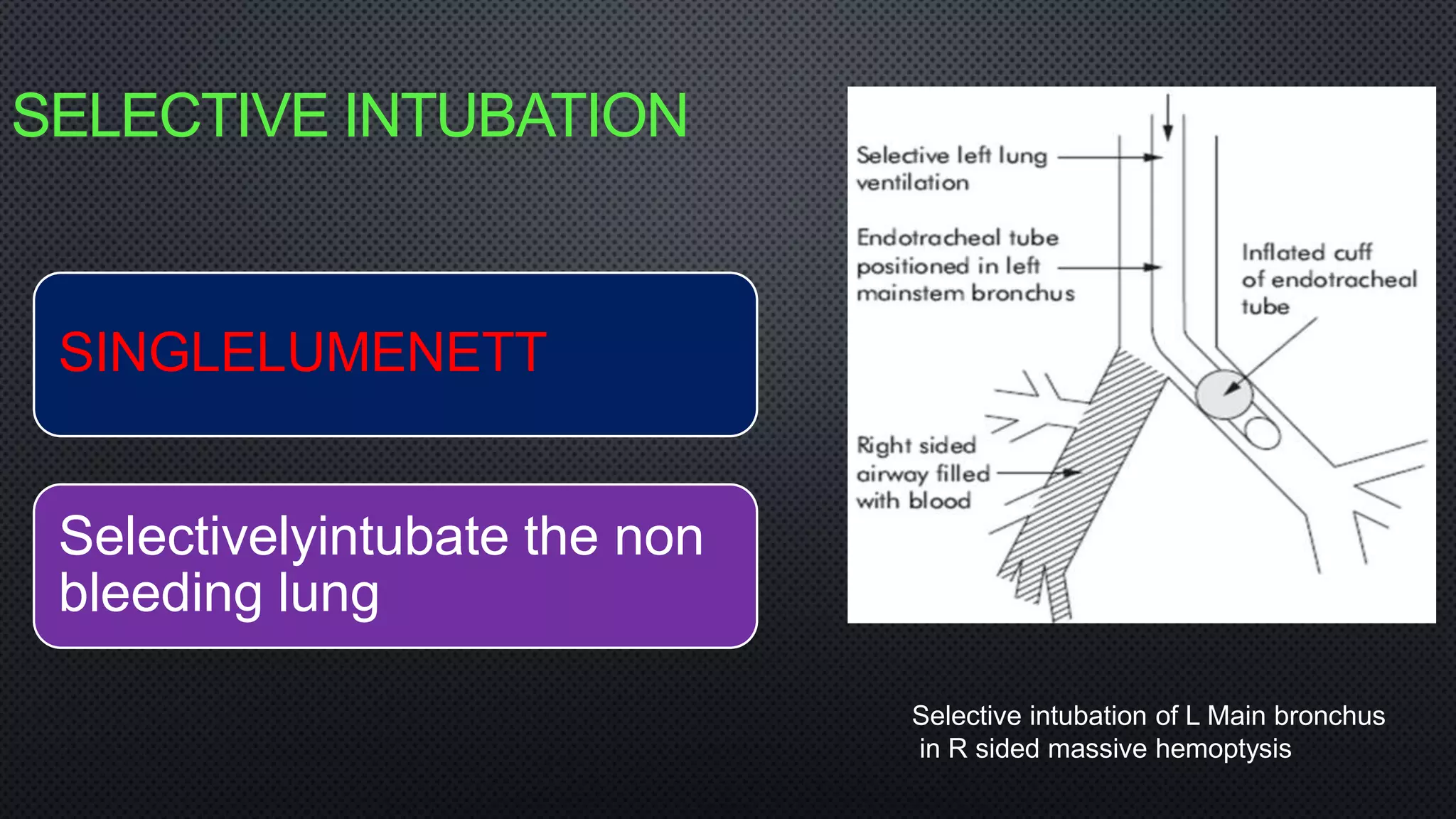
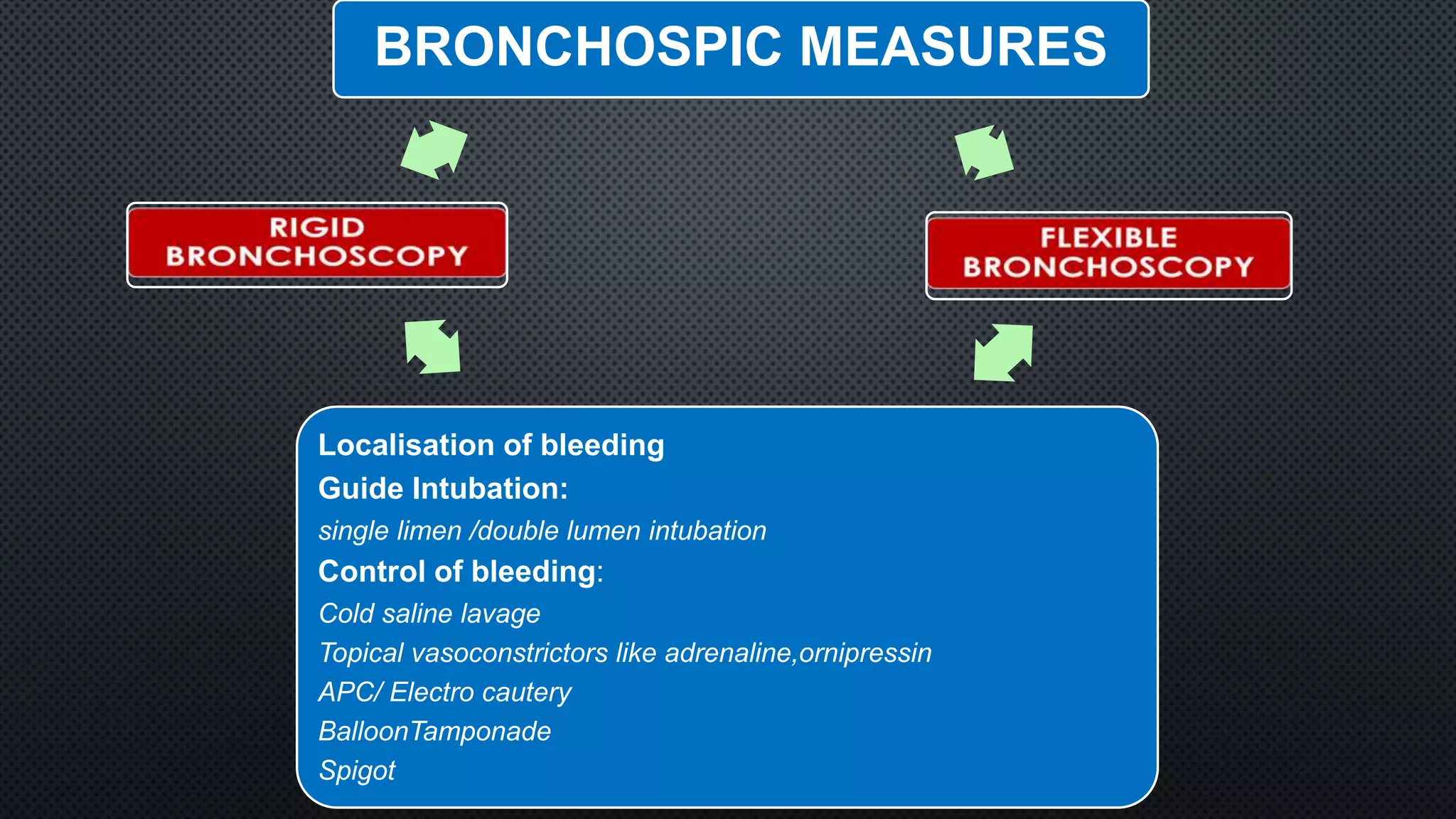
An 80-year-old female presented with a 2-day history of coughing up blood in multiple episodes of approximately half a cup each time. She had a history of hypertension but no other significant medical history. HRCT chest and CTPA showed a pulmonary arteriovenous malformation (PAVM) on the left side. She was initially managed with bronchial artery embolization (BAE) which failed to control the recurrent massive hemoptysis. She was then treated conservatively with blood products, oxygen supplementation, and medications. When hemoptysis persisted, surgical resection was considered but deemed too high risk. A second attempt at BAE also failed. The patient was eventually discharged after hemoptysis resolved