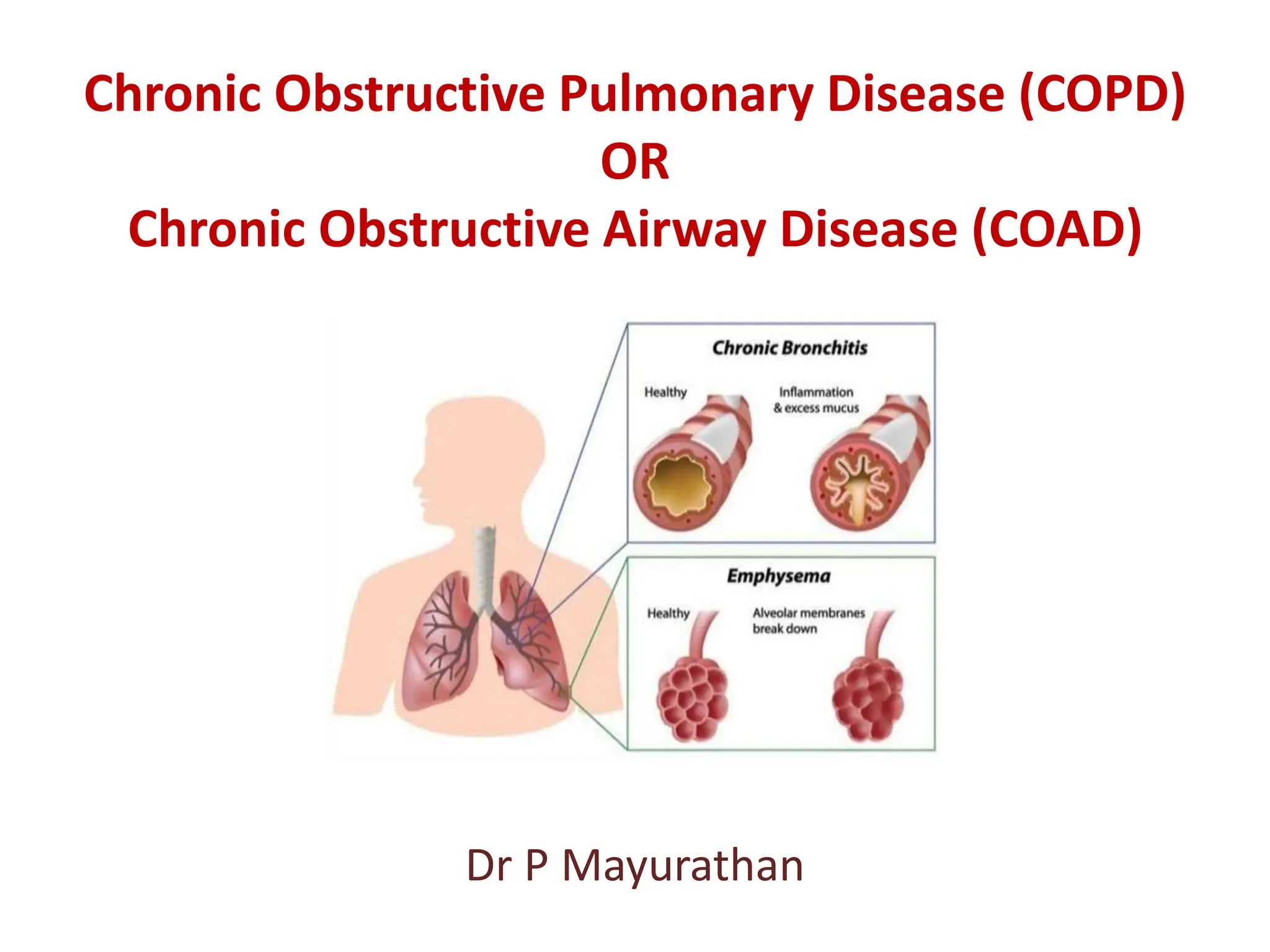
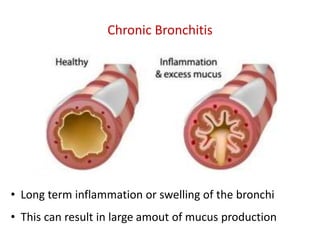
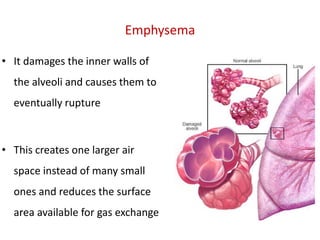
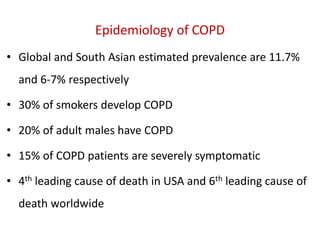
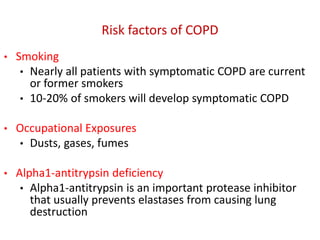
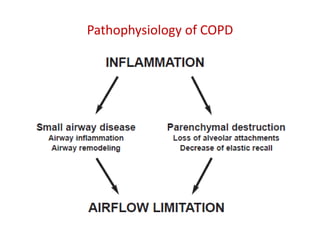
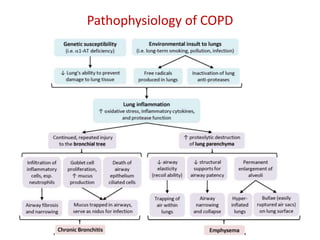
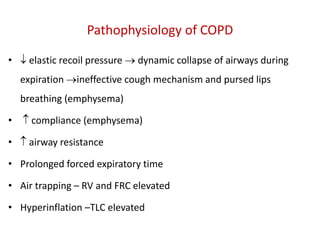
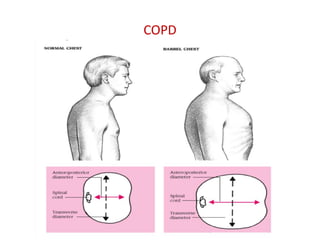
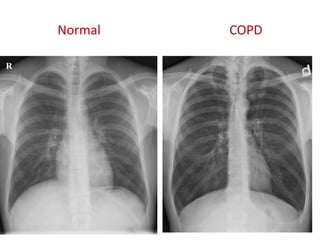
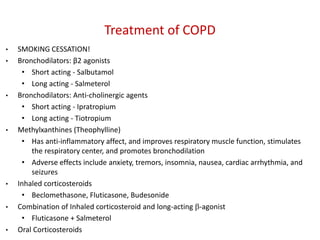
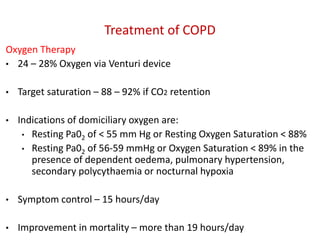
Chronic obstructive pulmonary disease (COPD) encompasses chronic bronchitis and emphysema, leading to airflow obstruction, chronic cough, and respiratory issues. Its prevalence is significant, with high smoking rates being a major risk factor, and it is the fourth leading cause of death in the USA. Treatment includes smoking cessation, bronchodilators, corticosteroids, oxygen therapy, and potential surgical options.