This document discusses ventilator associated pneumonia (VAP), including its definition, causes, risk factors, prevention, and treatment. Some key points:
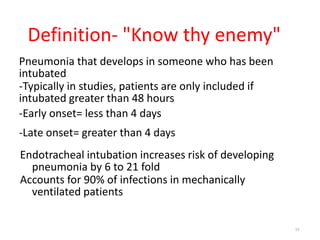
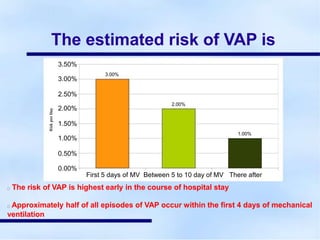
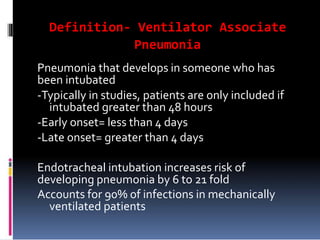
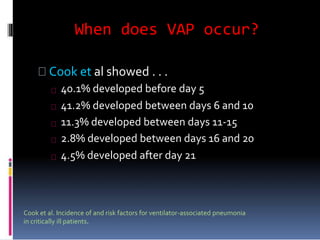
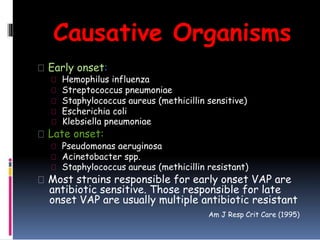
- VAP is pneumonia that develops in intubated patients and accounts for most ICU infections. It occurs in 10-20% of mechanically ventilated patients and has a high mortality rate.
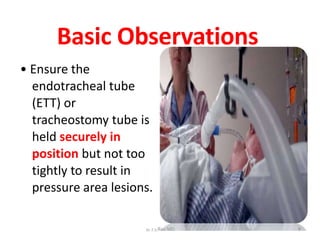
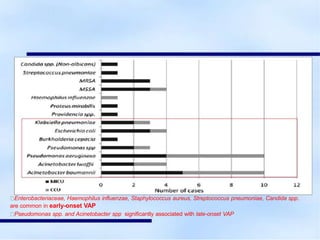
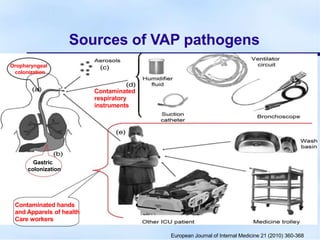
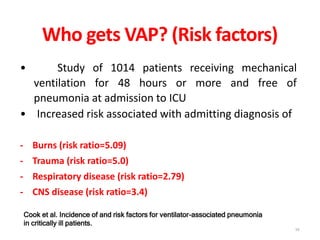
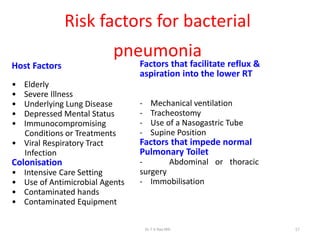
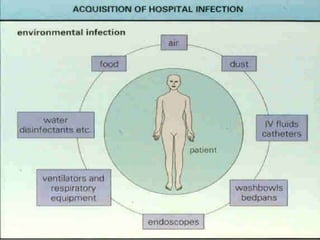
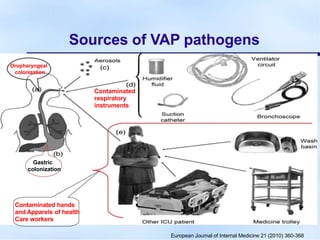
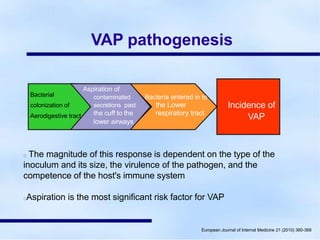
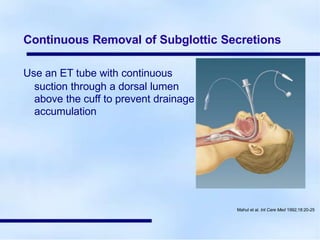
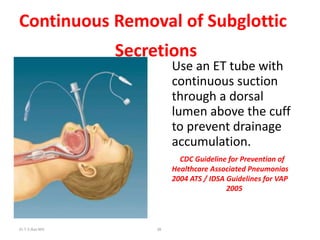
- Risk factors include underlying illnesses, suppression of immune system, and prolonged ventilation. Common causes are oropharyngeal/GI bacteria and viruses that enter the lungs through the endotracheal tube or around the cuff.
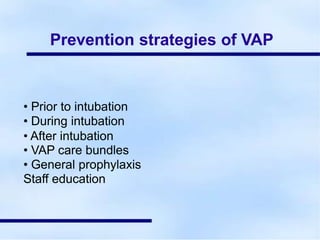
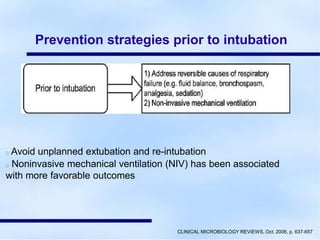
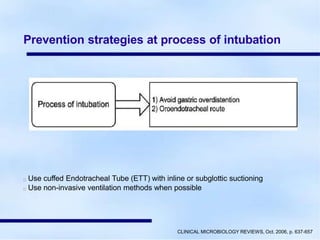
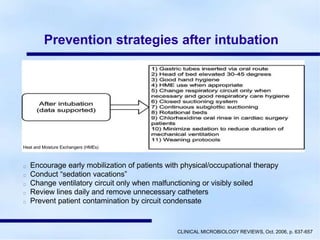
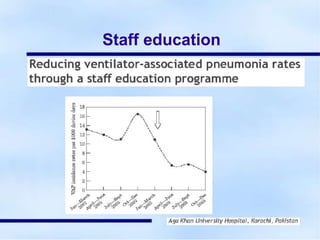
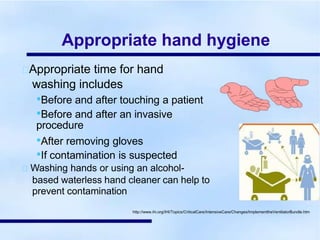
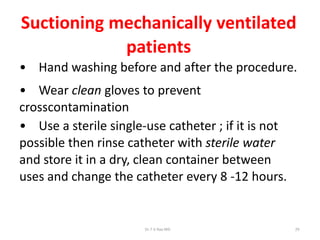
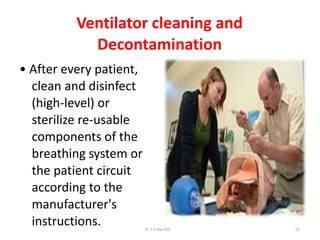
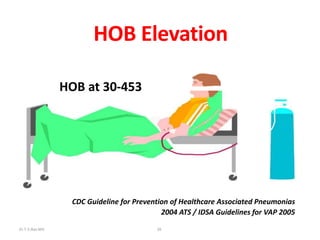
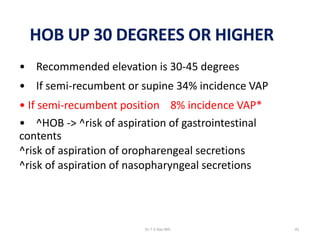
- Prevention strategies include following bundles like elevating the head, oral care with chlorhexidine, and stopping unnecessary devices; as well