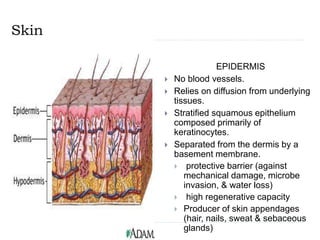
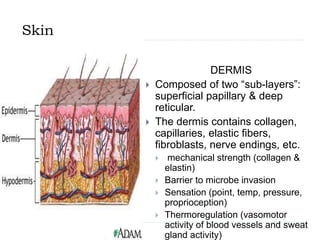
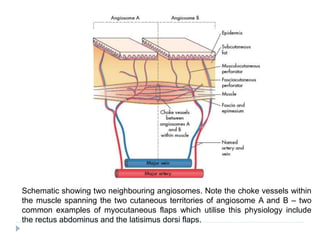
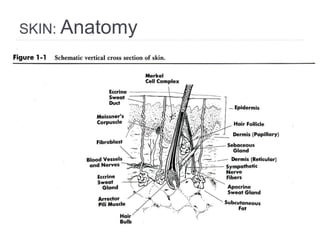
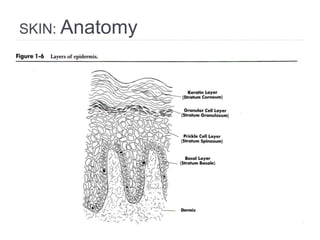
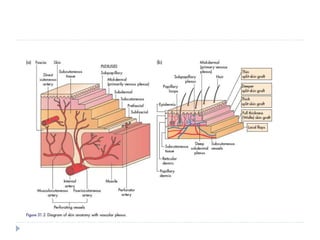
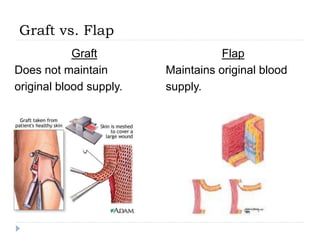
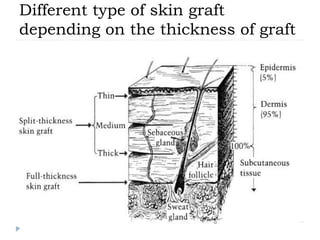
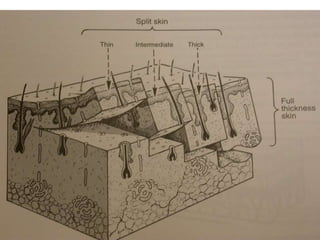
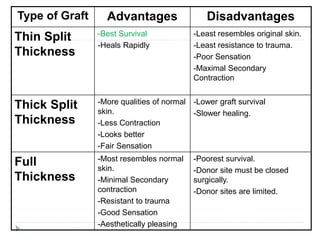
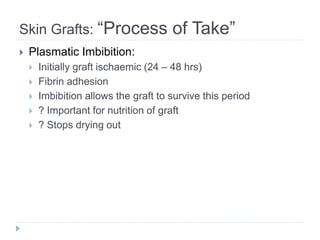
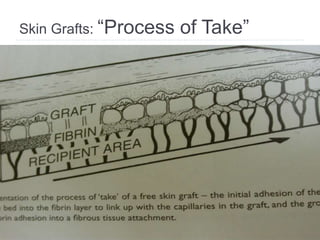
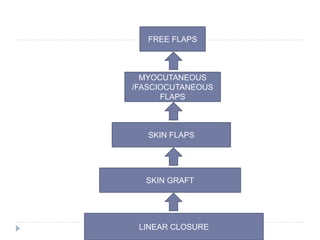
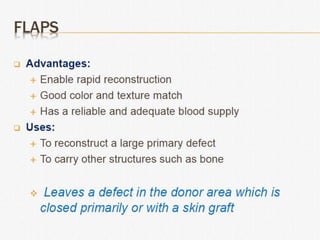
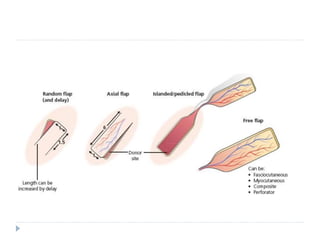
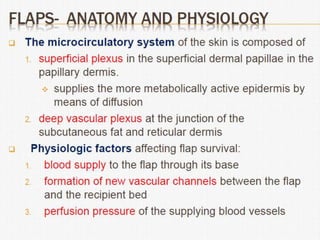
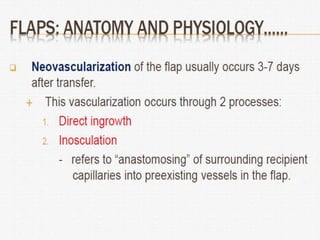
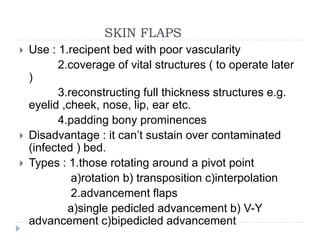
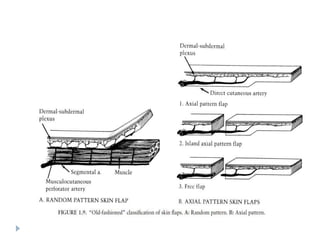
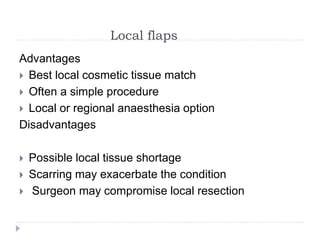
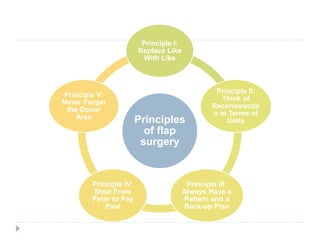
Plastic surgery principles aim to optimize wound healing through adequate debridement and resection while ensuring good blood supply. Scars should be placed carefully along lines of minimal tension and defects replaced with similar tissue. Meticulous surgical technique and consideration of donor site costs are important. The skin has two layers - the epidermis which acts as a protective barrier and the dermis which provides strength and sensation. Grafts do not maintain their original blood supply while flaps do, allowing flaps to bring their own vascularity to the recipient site. Careful technique and consideration of various factors influence graft and flap survival.